- Home
- About VCI
- Testimonials
- Contact Us
- Adventure CE
- VCI Programs
- VCI Ethical Values
- VCI Consultants
- Trusted Colleagues
- Initiatives to Watch
- Publications
- S@S Proceedings
- Design the Dream
- Veterinary Medicine & Practice
- Beyond the Successful Veterinary Practice
- Building the Successful Veterinary Practice, Volum
- Building the Successful Veterinary Practice, Volum
- Building the Successful Veterinary Practice, Volum
- Design Starter Kit for Veterinary Hospitals, 3rd E
- Healthcare of the Well Pet
- Promoting the Human-Animal Bond in Veterinary Prac
- Veterinary Management in Transition
- Veterinary Healthcare Services
- Veterinary Practice Management Secrets
- Newsletters
- Fortnightly Publications
- Fortnightly Articles
- Monographs
- Cat Sighting
- Pet Parent Sites
Veterinary Consulting International
(303)277-9800
www.drtomcat.com
|
Click below for the PDF's of the Fortnightly Articles or scroll down to read on current page: July 2015 - Mid- Month - Workplace Conflict Where does friction occur in the workplace? As a consultant, I get to see it in many forms: -Staff tasked to do a program when training has not been provided for "competency" -Staff seeing something that needs to be done, but they are ignored/stonewalled by owners -Providers making variances to the written Standards of Care without medical record details -Perception of inequality for vacations or shifts -Owner states a need/desire, but the team does not produce it in expected time frame -Veterinarians violate case management expectation(s) of attending provider -People come in late for shift, or take a prolonged lunch w/o telling anyone -People are empowered, yet ignored by decision makers over-ruling their zone of accountability -Lack of team work and/or respect toward others -Abuse of internal latitudes provided staff members
The above list is not all inclusive - there are many variations and tangents. In fact, while I find similar dysfunctions, the causes vary greatly. In most cases, the practice culture is caustic. When it isn't caustic, it is detrimental to harmony. FYI - I encountered a practice owner who wanted to realign the staff attention to process, but did not want me to address any programs. FYI - The doctor-centered practice is a common syndrome, causing production to stay less than $450k per FTE veterinarian, since team-based healthcare delivery was never taught in school, nor was leadership, business, or organizational behavior. FYI - I was visiting a practice where morning rounds always ended with each person answering the owner's recurring question, "What did you screw-up today?" FYI - I encountered a practice that had a large staff walk-out, and the locums and new staff were being handled with "kid gloves" - the owner/manager did not want to upset anyone, so the Standards of Care were not a consistency or even an expected standard. FYI - a common issue is low cash flow, or zero liquidity, and in most cases, the owner and/or management had no idea which programs were not producing and/or which providers were not embracing the SOCs and/or booking patients as jointly expected. FYI - I have seen practices where the patriarch has a negative feedback with staff at least once a day. Empowerment was not pursued for fear of the negative attack. Because of the negative feedback for independent thinking, even the smallest decision went to the patriarch and that often frustrated him.
The above list is not all inclusive either - there are many variations and tangents. In fact, while I find similar dysfunctions, the causes vary greatly. In most cases, the practice ownership has lost their focus on their vision and mission focus. There are a few consults that are really great - practices that want to go to the next level and want a savvy guide to help them and their teams. Many times, giving these visionary leaders the text on Servant Leadership excites them to seeing the many potentials available. Servant Leadership The concept of servant leadership has been around for ages, but it was not until Robert Greenleaf coined the term in 1970 in his paper, The Servant as Leader, that it became popular. Greenleaf defines it as wanting to serve first in order to ensure that other people's highest priority needs are being served. Servant leaders use less institutional power and control while shifting authority to the followers. Secondly, servant leaders have a positive effect on the least privileged in society; will they benefit, or, at least, will they not be further deprived? If inequalities and social injustices exist, a servant leader tries to remove them (Graham, 1991). Inversely, popularity does not equal leadership, while the four Fs are essential for becoming a good leader: fair, firm, friendly, and focused.
Servant leadership is both a leadership philosophy and set of leadership practices in that it emphasizes serving, while having ten principles (Spears, 2010) to guide the servant leader. In my text, Building the Successful Veterinary Practice: Leadership Tools (Volume 1), Wiley/Blackwell Publishers, I provide 14 leadership skills as we have presented them in high adventure leadership courses in the Rockies. I sincerely believe leadership is within the grasp of most practice owners, yet many seem hung up on management only. Leaders seem to engage and influence people through four mechanisms: what they do (role modeling); what they say (effective communications and narratives); systems and processes (tracking Key Performance Indicators, staff selection, and strategic budgeting); and the practice culture (Core Values, Standards of Care, Continuous Quality Improvement (CQI). Often leadership only focuses on the first two mechanisms, yet most stuff-ups occur because of neglect of some aspects of the last two. The attached article on workplace conflict attempts to put it into a working perspective. I hope you enjoy the adventure. I really enjoy helping a practice move to the next level. While the full-year consult allows me to return quarterly (and keep the practice on track), I do offer smaller bites for practices that have a lesser desire (/vci-programs.pml). I lower my prices after the GFC to make it easier for practices to access my services. This year I am commuting to the USA via San Francisco, Denver and Chicago for on-site consults, and new clients who marry up with the quarterly visitation schedule, can share in expenses (e.g., car rental, lodging, food, and a percentage of the air expense). The above-linked various consult offerings are categorized on "time-based" parameters, and like every consult I do, they are tailored to the practice's needs/desires; boiler plate consulting does not work, nor does "phone-it-in" styles, the real "rubber on the road" insights/programs require me to be on-site. The scope becomes more limited with shorter periods, but in some cases, there is just a tweak desired. The first phone call is always a courtesy - try it, you may like it. :>)
Tom Cat >*-*<
Thomas E. Catanzaro, DVM, MHA, LFACHE
P.S. Please review the VCI SEMINARS AT SEA 2015 (/site/view/214832_.pml ), departing New Orleans after Thanksgiving for 7 days in the Western Caribbean. You'll never have another continuing education opportunity where faculty are available for 7 days to explore specific practice tailoring questions/concerns.
July 2015 - Winning Attitude Okay - what is stuck in my craw this week? I have been battling "sound byte" leadership session, sometimes from weekend courses that "feel good", sometimes from texts that are "easy reads" and more often from seminars where the speaker can pontificate a leadership thesis, but has never had it make it work in an alien environment or different practice culture. This new breed of consultant, "this worked for me in my practice" most often ignores the long and laborious total efforts required to build the culture where ideas can land on fertile ground.
Add to that the current journal expectation that meaningful messages can be delivered in 1500 words and we can see the formation of frustration factors. Veterinary schools have not taught business (and students have not really enjoyed the meager efforts that have been tried). Also, most veterinary schools have not taught leadership (and most students have not really enjoyed the life experiences to appreciate the need). Add to this the use of a team-based healthcare delivery culture, seldom seen in the practices of old and not that common with today's practice owner who wants to keep "tight reins" on the practice flow - a culture of distrust develops that most owners do not even understand. Most new graduates do not understand how fragile the team confidence is when they vary from the Standards of Care, but then, most practices do not have a written Standards of Care for Risk Level 1 animals that are inviolate!
What is the solution? To transition a practice culture, the practice owner and manager must first transition their approach to human dynamics. Read and understand three critical texts:
1) QBQ! The Question Behind the Question: Practicing Personal Accountability in Work and in Life, by John Miller 2) How To Get Your Point Across In 30 Seconds or Less, by Milo Frank3) Crucial Conversations: Tools for Talking When Stakes Are High, by Patterson, et.al.
When I wrote the text, Building The Successful Veterinary Practice: Innovation & Creativity (Vol 3), I put a STOP SIGN and challenge in the preface. I also have an empty iceberg on every right hand page (Vol 1 and Vol 2 had applicable quotes in the iceberg), and prompted the reader to put their key point into the iceberg from every two pages of reading. Every chapter ended with a mind map charter, and an early format to be completed, to be completed by the reader. As I travel around veterinary practices, I often find my three volume starter set on the bookshelf. I open Volume 3 and see if they have done anything I suggested . . . needless to say, it seldom has been done at any level of attempt! So when I say "read and understand" the above three basic texts when you embark on the culture changes needed for team-based veterinary healthcare delivery, I concurrently accept that most practice owners and veterinarians think they know better, although they have never practiced in a multi-tasking, team-based, environment.
How do I know this? In 2007, we put the landmark text into the VIN Library for FREE download, THE PRACTICE SUCCESS PRESCRIPTION: TEAM-BASED VETERINARY HEALTHCARE DELIVERY //www.vin.com/Proceedings/Proceedings.plx?CID=TomCat2007&O=Generic. I say landmark because in 2014, AAHA chose that subject as their initiative. Most people accessing the free site and data (500 pages with 18 appendices) complained they had challenges in implementation. Upon follow-up, they had cherry picked the ideas, and did not spend the time in basic orientation & training, or even the systems and schedules needed to make it work. This is not the gimmick of the week - it is a total 24/7, 365 commitment! It is not the 1500 word sound byte of the journals. It is not a 90-minute "I did it once" seminar discussion. I have been in 2000+ practices and seen good implementation as well as the bad. Picture a practice owner investing money in team-based leadership training (sometimes he did not attend) for key staff, then tasking them rather than asking them about initiatives. The usual answer when asked "why the tasking?" is usually, "THAT TAKES TOO LONG TO ASK".If you do not want to read references, you could invite me in (/vci-programs.pml),but understand you must be willing to change, since what you have is what you built. If that is not feasible/acceptable at this point in time, you may want to consider visiting the New Orleans port for VCI Seminars at Sea 2015 (/site/view/214832_.pml) where you have FIVE consultants for seven days - plenty of time to pick their brains one-on-one while cruising in the Western Caribbean 29 Nov to 6 Dec (if you decide on a consult from there, I credit back to your account with the seminar registration against the consult fee).
Trust me - changing your practice culture to be a multi-tasking, team-based, veterinary healthcare delivery system is not just a snap of the fingers nor a "I said so" effort. That is why on a consult I build step-by-baby-step monthly Action Plans . . . and why as I track the KPI's monthly . . . we also discuss the monthly Action Plans. Hint, while I do return quarterly, if you select not to keep me informed with a monthly KPI an Action Plan submission, that is YOUR choice. I have learned that I can never try to do more than what you are willing to do.
Think about what you want to experience in 3-5 years. Many of the KPI aspects provide immediate program-based rewards, but it is an integrated leadership team that will allow it to continue and mature as you kick back and relax.
Tom Cat >*-*<
Thomas E. Catanzaro, DVM, MHA, LFACHE
|
|
HIGH RISK HIGH FEEDBACK “Tough-guy Macho” [e.g. police, surgeons, entertainers]
|
HIGH RISK LOW FEEDBACK “Bet Your Practice” [salesperson, office equipment, retail] |
|
LOW RISK HIGH FEEDBACK “Work Hard/Play Hard” [oil companies, military]
|
LOW RISK LOW FEEDBACK “Happy with Status Quo Processes” [bank, insurance, government] |
No successful organization will be one type only; they will blend all four types.
PREPARING THE PRACTICE FOR CHANGE
Building support for change requires “internal selling”, discussed at length in the VCI Signature Series monograph, Leadership Action Planner, available from the VIN Bookstore. There is also a VCI Signature Series monograph, Strategic Assessment & Strategic Response, available from the VIN Bookstore. The VCI Signature Series monograph, Models and Methods, available from the VIN Bookstore, shares some insights on “why” new programs require new metrics. A practice that is unwilling to
modify their metrics is a practice that is usually destined for regression after the Strategic Planning retreat.
The first item is to get a team understanding of:
A2 = G2
If you Always do what you have Always done,
you are going to Get what you always Got.
In most cases, the “unselling of the old” and “selling of the new” are two separate leadership campaigns, yet most veterinary practices do not spend the time needed in doing either. However, these two tasks are interdependent and inseparable. The process must ensure the team members are convinced that the times have changed, the status quo will not ensure the future, and the transition process for change is needed. In practices where innovation has been encouraged, where outcome goals were Zone accountabilities, and change efforts have been rewarded, strategic assessment and response become easier.
In practices with a strong sense of mission, vision, and/or purpose, where inspired leadership motivated others to pursue the long-term goals of the zones and/or practice, formal planning mechanisms have been viewed as less important in the implementation of the transition to change. If you read the characteristics of entrepreneurs, most of them have no plan(s). When you put a plan on a piece of paper team members feel they cannot change it or adjust it, so you have lost the ability to have a strategic response to a dynamic strategic assessment.
On consults, I try to convince practice owners that they owe the staff members the WHAT and WHY of new ideas/programs (basis of the written SOC). They then need to empower the zone teams to develop the WHO and HOW (which takes a bit longer than a doctor-centered edict). After the Zone teams have the WHO & HOW figured out (e.g., protocols), the zone coordinators and leadership come together to jointly discuss the WHEN, which includes milestones and success measures. Training time precedes any implementation effort.
PACING THE CHANGE
On my year-long consult planning, I do a month-by-month step-by-baby-step process checklist, and ask the practice leadership to pace themselves, and keep me posted on their progress. I provide augmented set of metrics, and integrated spread sheets tailored to their practice, with the request to submit the documents with updated data monthly for my review and feedback. Even with these custom-built tools, there are practices that will not alter their metrics, so they do not complete the spread sheets, and feedback becomes minimized . . . change is minimized concurrently.
- Identification of “hot buttons” (key interests) of various staff members, and the strategic empowerment through directed training toward outcome goals, underlies many new program initiatives.
- Knowing when to act and when to delay is essential in managing the transition process for change initiatives.
- Change-makers must often wait for a propitious moment and prepare to take quick action when the time is ripe.
- Deciding whether to make an immediate attack or move more slowly is usually more a matter of management style than planning policy.
CRITICAL ELEMENTS OF MANAGING STRATEGIC RESPONSES
Great leaders move others to action through the force of their personalities, their style of management, the in-house educational process, and the use of Task Forces to flesh out ideas and build coalitions for their support. That said, there are some critical elements for managing strategic assessments and strategic responses:
- A committed, dynamic, creative top management group which is able to communicate its vision and goals to others.
- Established system of task force delegation and ad hoc group empowerment to move ideas into action and/or gain broader consensus.
- A practice climate that is ready for change, or at least is capable of responding to external and internal stimuli.
- History of team commitment through participation and involvement.
- Maintains a system that is ready to reward innovation, excellence and encourages people to take risks, while NOT penalizing them for honest failure.
- Recognizing when a more participative style is necessary and willing to sacrifice management prerogatives and control to further the team approach.
The half dozen elements above need to be “in effect” before a strategic assessment group session is formulated. The team members must believe their contributions are appreciated, promises will be kept/honored, and that they have been empowered with CQI (continuous quality improvement) within their sphere of influence. If you cannot see yourself committing to the above six elements in daily operation, then please do not commit to a team-based strategic assessment and strategic response effort.
January 2015 (mid-month) - Leading Your Team & Charisma in Leadership
The New Year- time for making those resolutions that will too often be forgotten by February. A survey of 1000 Australians found 69 per cent of us intend to make at least one New Year's resolution. And while less than a quarter of us will stick to achieving our goals, there is a secret to succeeding. A year-long study at the University of Hertfordshire in the UK found the key to keeping your resolutions varies according to your gender. For men, setting specific realistic goals, such as "lose five kilograms by April", rather than just "lose weight", is best.
Women should share their resolutions for the coming year with others, as, according to study leader Professor Richard Wiseman, "women benefit from the social support provided by friends and family". "If you halve your goal you'll be more likely to achieve it," dietitian Kate DiPrima says. "Instead of saying you'll exercise every day, make a commitment for three times a week. This way you'll have a sense of achievement rather than failure."
"The greatest danger in times of turbulence
is not the turbulence; it is to act with yesterday’s logic."
Peter Drucker, Management Guru
In a veterinary practice setting, it means looking at your written Standards of Care (SOC) and comparing them to the historical KPIs (e.g., key procedures per 100 transaction). It also means a time to assess the SOC document for long needed upgrades to the WHY and WHAT of that document. The WHO and HOW are protocols that belong to the staff, driven by the clear and concise written SOC document. WHEN is the time after the nursing staff has done the WHO and HOW protocols to meet with the key providers and establish time lines, success measures, and training commitment needs.
PLEASE - keep it real. Stating, "We will make 15% more money!" has nothing the staff can grab onto and work on to achieve. If you state, "We will book 10% more DG1+ dentistries each month, compared to same month last year.", that is something everyone can work toward. The RECOVERED PET and RECOVERED CLIENT PROGRAMS (10% more each month than the same month in the previous year) are also great goals for the front desk team.
So saying that about resolutions and resistance, I drafted the attached article to talk about change, transition, and the paradigms that prevent both. I hope it is helpful for the new year - and maybe, just maybe, a few of you will decide you need a savvy veterinary guide. My consulting programs are listed at www.drtomcat.com - also, unlike the newbies who "say" they are consultants, my philosophy is well established in the 15+ books I have published (most are available from Amazon.com, except the two new ones that are in the VIN Library for FREE download), and the 30+ monographs in the VIN Bookstore.
I wish you the very best in the new year, and hope your change transitions are exciting, fruitful and filled with wonderment.
Tom Cat >*-*<
January 15, 2015
LEADING YOUR TEAM
Thomas E. Catanzaro, DVM, MHA, LFACHE
Dipomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com

Graphic built by VHMA
"The objective of leadership is to accomplish the mission in the minimum time and with the maximum balance of individual needs."
Dr. T. E. Catanzaro
Profit-based performance standards require effective leadership to make them work as positive motivators. The ultimate objective of leadership in any organization will always be the successful accomplishment of the goals and objectives of that organization. In veterinary practice, Veterinary Consulting International has defined the ultimate veterinary hospital management objective as follows:
TO ENSURE QUALITY HEALTHCARE DELIVERY FOR EVERY PATIENT PRESENTED WITH AN ACCEPTABLE RATE OF FISCAL VALUE AND ADEQUATE QUALITY OF LIFE FOR THE PRACTICE AND ITS STAFF WHILE ESTABLISHING A CLEARLY DEFINED AND CLIENT-PERCEIVED VETERINARY SERVICES MARKET NICHE IN THE COMMUNITY.
In striving to achieve this goal, the leader must accept full personal responsibility for all his/her decisions and must continually assess the situational environment in which the practice operates. Continuous quality improvement (CQI) requires that every member of the staff is accountable for the daily activities and pride in the tasks performed; the client perceives the outcome of that effort as quality care. Using profit-based performance standards is one method to recognize the staff's contribution to the hospital's CQI program.
STYLES OF LEADERSHIP
Too often leaders focus their efforts on short-range goals at the unnecessary expense of their subordinates (the team is subordinate to the leader, but do not need to be made to feel that way). In the long run this can be detrimental to both the staff and the practice. Effective leadership is accomplishing the mission with a minimum expenditure of personal time and effort and an appropriate balance between practice, staff, and individual needs and goals.
Leadership ability becomes increasingly important as the practice team expands. When the practice becomes a multi-practitioner healthcare delivery system, leadership becomes a prerequisite for team building and success. While there are many styles of leadership, shades of grey in the spectrum of good approaches that vary with the situation, most all can be classed as either directive or nondirective leadership methods. The directive leader tells the staff exactly what to do and lets them know who is the boss. Group members have the secure feeling of knowing exactly what is expected of them. Nondirective leaders seek the opinions of team members, consult with them in planning and decision making, and sometimes, on non-health care issues, even put ideas to a democratic vote.
MATCH THE CONTEXT
Neither approach is appropriate at all times. In general, directive styles will be more appropriate in lifesaving situations and with starter-level employees, and a more participative style in practice management situations and with professional and paraprofessional associates.
Summarizing research, models, and theories developed by a variety of social scientists, Claremont McKenna College professor Dr. Chemers gives this advice: "If your subordinates do not have the knowledge necessary to perform the task, or if their attitude is such that they lack commitment to the goal at hand, a directive approach is warranted." The most common example of this situation is the chemotherapeutic regimen for a patient where the drug, dose, and duration and administration is dictated by the veterinarian.
Of course, even the best veterinarian doesn't always have a clear picture of what the most desirable course of treatment should be. You may need a colleague's perspective or the staff's ability to provide subjective information on the case or client; here, participation is called for. When a veterinarian is nondirective, it is more likely that the team members' intellectual abilities, years of practical experience, or technical capabilities will contribute to the task. This is especially true for challenges in practice management that deal with client bonding or improving productivity.
The participative style has some important bonuses. It makes team members feel autonomous -- a proven motivator for many personality types -- and it gives them the opportunity to develop their skills. In deciding between the two schools of leadership, also consider the bottom line -- "Can subordinates be expected to energetically implement a management decision if they didn't participate in making it?"
A COMPATIBLE FIT
If one style or the other feels uncomfortable to you, don't be surprised. Many theories assume that any person can be equally adept at any behavior; this just isn't the way it is. A considerable body of research shows that leaders have personal styles that they are more comfortable with and that they habitually use.
If you are the type who is very concerned about relationships, about harmony, and about acceptance by the staff, you will lean toward the participative styles. They place greater emphasis on morale. If it is very important that people like you, there will be difficulty with the directive styles of leadership. On the other hand, if there is a high need for order and a very strong desire to accomplish a task efficiently as possible, you will find frequently that the directive approach is favored.
Knowing which end of the spectrum is preferred by your colleagues or the practice owner can help you work with them more successfully. If you are the associate and the practice owner is highly directive, you can depersonalize and defuse most situations instead of taking his personality as a personal affront. More importantly, if two veterinarians are both directive in style, there will be conflict about whose directions are best. Both want an orderly practice environment -- but based on their own order. If both veterinarians are participative in nature, they may want to avoid conflict so much that they don't control problems and, therefore, waste a lot of time.
People need to understand their own inclinations, the partner's style, and if employed, the leadership style of their boss. If attention is paid, situations can be recognized before they reach an impasse.
Regardless of styles, the secret is to communicate effectively. This means that information is given AND received in each exchange. Brains and ambition are hard to recognize and reward if they are muffled by lackluster or annoying verbal traits. It doesn't matter how brilliant or sincere an individual is; if the message doesn't come across verbally, it will be lost.
THE FILTERS
Information is processed at various levels of understanding. Based on the mind-set of the listener, it flows through the experiences of the past and distortion is added. Every person has these filters, so additions and deletions are made based on interpretation. Some of the more common filters seen in practice leadership situations include:
* What the leader believes he/she "heard", either verbally or in writing. Clarification is seldom discussed.
* What the leader believes the staff should know, for their own good or for "protection" of the practice.
* What the leader believes the staff wants to hear, regardless of the practice needs or environmental situation.
* What the leader thinks should be "toned down" or "built up" for the benefit of the receiver. Facts are mediated.
* What the leader's values and attitudes do to the information; the bias of prejudice and personal ethics.
* What stress or stresses the leader is operating under, at home or in the practice.
* What importance the leader attaches to the information, the validity of perceptions other than their own.
* What the leader feels at the moment that the information is being received or when passing the information to others.
When we consider the filters that information must pass through at each level, it is understandable that distortion, dilution, or total loss of understanding occurs. Do not misunderstand these comments. After all, it is the leader's job to overtly filter messages in order to clarify them or add to them as required. The leader, however, should not allow personal feelings and stresses to filter communications inappropriately or covertly.
The downward flow of information has the practices' seal of approval behind it; a kind of gravity flow exists. On the other hand, feedback is critical to ensure communication has occurred; remember, both the giving AND getting of information is essential for effective team communications. The average veterinary healthcare delivery team also has filters installed in the communication process. Many of the "staff filters" are more severe and cutting than those applied to downward communication, making meaningful feedback more difficult. Some common filters that staff members apply to upward communications are:
* The notion that any opinion in opposition to the bosses' idea is "negative thinking" and therefore bad.
* The notion that practice teams always gripe, and you should only worry when they don't.
* The belief that the information is unimportant and that the originator does not have the big picture in mind.
* The belief that the veterinarian(s) are not interested in the paraprofessional perception.
* The belief that you will get into trouble for passing along this type of observation or information.
* The belief that the information will reflect adversely on you, your ability, or the staff effort.
* The belief that the practice manager/ownership only want to be told the good things and not the bad things.
Do not think that all filters are bad. Some filters serve a useful purpose. You should try to solve problems, or when addressing a problem, offer at least two alternative solutions. You need to take the appropriate action, try the best alternatives, and pass on the significant information. Whining is not constructive communication. The acid test is to ask yourself whether you would need or like to have the information if you were in the leadership position. Only pass the information on if the answer is yes.
THE BRIDGE
Some guidelines for communicating more effectively with either style of leadership are:
* Keep it short, simple, and direct.
* Word your questions so that they will elicit a "yes" response; the position is then associated with the positive.
* Suit your message to the audience.
* Use words like "let's" to automatically associate yourself with the team.
* Use a story or anecdote as a window. Construct a vivid scenario of "what if" or "when" to make the team imagine the events already occurring.
* Using words like "right" or "truth" puts your position on the positive side of a debate.
* Know when not to speak. A dramatic pause after a particularly important point will stress your sincerity. It also allows you to evaluate the reception. If negotiating, present your case then leave in silence.
Improving your own communication skills to meet the needs required to cope with varying leadership styles is only smart business. Select those things you can effect, and do your best to be all you can be with those things you can influence. Do not spend great amounts of time fretting over things that you cannot influence. It makes for a far better practice environment.
MAKING IT COME ALIVE
This is the time of practice change . . . ambulatory medicine lone-doctor practice paradigms have been modified by expansive multi-doctor facilities, linear scheduling has given way to multi-tasking, doctor-centered decisions have yielded to client-centered planning, curative medicine training has become secondary to wellness services for companion animals, and the list goes on and on. The mission focus is no longer centered on just doing a great veterinary job on medicine and surgery, and with the new Pet Wellness Programs being promoted in many venues, savvy leadership must restate the mission focus to excite the hearts of staff and clients alike, something to the effect:
Client-centered patient advocacy to enhance and extend
the quality and duration of the companion animal’s life.
Through an awareness of the filters and barriers in the practice communication systems, a leader can decide which communication system can be used, how to reduce the effects of the filters, and where to look should breakdowns occur. Good communication does not just happen -- it must be developed and maintained be each and every team leader.
An important facet of any leader's responsibility for developing and maintaining effective communications is that of daily coaching and counseling. The veterinary healthcare team wants to be better; they want to give the best to the clients and patients. Communication is the most significant means of influencing a team member's behavior, their image of self-worth, and their participation in the practice's goals and objectives.
--------------
Charisma in Leadership
Thomas E. Catanzaro, DVM, MHA, LFACHE
Diplomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com ; www.drtomcat.com
CHARISMA DEFINITIONS, as a noun:
1. Theology . a divinely conferred gift or power.
2. a spiritual power or personal quality that gives an individual influence or authority over large numbers of people.
3. the special virtue of an office, function, position, etc., that confers or is thought to confer on the person holding it an unusual ability for leadership, worthiness of veneration, or the like.
As you walk into the bookstore, and wander down the business text aisles, please note the number of texts on leadership and management. This is proof-positive that there is no one set answer for the best outcomes. The first text I published, Building The Successful Veterinary Practice: Leadership Tools (Volume 1) Blackwell/Wiley Publishing, was caused by my consulting team taking me to task because the first book I drafted, Building The Successful Veterinary Practice: Programs & Procedures (which became Volume 2) referred to leadership and teams, but did not give the basics. Volume 1 has 14 leadership skills which can be taught, but the assimilation into daily life is much more difficult than just reading the text.
Most students of team-building have long acknowledged that many aspects of leadership remain a mystery. I believe that both TRUST and RESPECT are critical organizational behavior elements of leadership, and another such attribute is the concept of “charisma.” Charisma has been described as a quality that enables leaders to influence others, to attract followers, and achieve remarkable outcomes beyond that of any individual.
According to the late Peter Drucker, leadership was all about delivering results. While the nature of these results may vary from one organization to the next, all organizations exist to bring about some form of desired result. As a leader, you have been charged with the challenge of delivering those results that truly matter within your organization, whether it be a veterinary practice, a family, or a volunteer organization. And be certain of this, it is not just any result, but something that others consider extraordinary — something that pushes and passes the boundaries of normality. Drucker’s incisive insight into the nature of leadership was quite empowering to American leadership for many decades. As a leader, you have many demands on your time. If you are clear about the results you want to achieve, you can focus your efforts and limited time on those activities that contribute the most to delivering results. Yet, while Drucker’s view provided a focus, it failed to differentiate between a star individual and a great leader. To be effective at work, both staff and their leaders need to be focused on achieving the best results that they can. The best player on a team does not always make the best captain or coach. Why? Because leaders are concerned with delivering results through the IMPACT they have on the attitudes and actions of others. Any success as a “leader” is all about the impact made on those that have been led. Understanding that leadership is all about the impact you have on others is central to enhancing your own leadership effectiveness. The central question becomes, “How can I have more of an impact on others?”
There was an interesting book published in 2009, Unlocking the Mystery of Inspiring Leadership, by Zenger, Folkman, and Edinger, that started as follows:
Mysteries Block Progress
About five percent of the population will develop a stomach ulcer at some time in their life. For many years, it was assumed that the cause of stomach ulcers was excess acid in the stomach that came from stress, diet and general lifestyle. The wall of the stomach became inflamed and sometimes this was so severe that the stomach would be perforated, in which case it often became a bleeding ulcer. Physicians recommended that patients eat bland diets and avoid stress because excessive stress and the production of stomach acid were known to go together. Some foods were thought to either be more acidic or to cause the stomach to produce more stomach acid.
Then in 1982 two Australian scientists discovered that the bacterium “Helicobacter pylori” was the cause of more than 90% of stomach ulcers. Discovering that the basic cause of ulcers was something totally different than had been assumed led, of course, to radically different treatment. Without that discovery we can only assume that physicians would still be prescribing bland diets and stress avoidance for ulcer patients
A Leadership Mystery
Let us now switch to a totally different arena, the study of leadership. Despite all the research that has taken place about the nature of leadership, practitioners and scholars have long acknowledged that many aspects of leadership remain a mystery. What’s more, we have described these mysteries in terms that readily concede that it they are something that we simply do not understand. We would like to address one such mystery.
Often, leaders have been identified as possessing some remarkable quality that sets them apart from others. This quality enables them to have a powerful influence on others. It causes people to be attracted to them. It enables them to achieve remarkable outcomes. We have labeled this quality “charisma,” coming from the Greek word meaning “gift.” It was thought that this quality was a gift that was bestowed upon some and not others. No one knew where it came from. Unlike other leadership skills such as giving compelling oral presentations or delegating, no one attempted to teach charisma.
But having given this quality a label allowed observers to say things like, “Well, the reason she has been so effective in her role is that she’s charismatic.” Others hearing this would nod their agreement and concur. Everyone pretended that they understood what was meant. In truth, no one had the faintest idea what ”charisma” was, other than that there was a special quality this person possessed.
For those involved in leadership development the questions were even more profound. Not only is there a question of understanding it and being able to define it; but more importantly, can it be learned or acquired? Can it be measured? What kind of impact does it really have? Is there one way that charismatic or inspiring leaders behave or does charisma have several “flavors?” What the authors discovered after assessing 14,500 leaders confirmed, “expertise, inspiration, and motivation” were the key factors from followers for defining leadership competency. Inversely, when assessing leadership competency, followers (managers, peers, and those who report to them) poor leaders got the lowest scores in these same areas.
Like most researchers, these three authors loved to make lists of the feedback they received, and defined three major areas which set inspiring and charismatic leaders apart:
AREA ONE – ATTRIBUTES (broad and general qualities)
1. Role Model – excellent examples of WHAT they want others to do
2. Change Champion – constantly challenging the organization to change
3. Initiative – a driving force to make things happen for the better (status quo goals were considered NOT INSPIRING).
AREA TWO – BEHAVIORS (six discrete, actionable behaviors used by inspiring leaders)
• Stretch Goals
• Clear Vision and Direction
• Effective Communication
• Developing People
• Teamwork
• Innovation
AREA THREE - EMOTION (the contagious nature of the positive mental attitude)
? Evoking a similar and positive emotional response in others
? Leaders position acts as an accelerant to any emotional contagion that occurs, altering the organizational behavior into an energy flow (inversely, negative emotions of any type shut down the organizational culture’s energy flow).
BACK TO THE VET TRENCH
The data from multiple authors indicates that inspiring leaders utilize a variety of ways to connect with those about them (Hershey & Blanchard called it Situational Leadership, which I thought was a great term, so included it in my 14 leadership skills). The good leaders don’t do just one thing. Indeed, it is the combination of several approaches that lifts people to a higher level: Great leaders use five or more, and usually vary the approach with the people involved, project goals, and organizational culture level (for more information, see the VCI Signature Series monograph, Human Resources & Organizational Behavior, available from the VIN Bookstore, www.vin.com)
In the 500 page (18 appendices), March 2008, VIN Press text, The Practice Success Prescription: Team-based Veterinary Healthcare Delivery, which is now available for FREE DOWNLOAD from the VIN Library (www.vin.com), I shared both a SYNERGY MODEL, and LEADERSHIP PRACTICE IMPACT MODEL . . . Training To Trust is the first step in the SYNERGY MODEL, and Building Mutual Respect is the second step. As far as the perception of clients – they really don’t care how much you know until they know how much you care! The other favorite quote I use on consults is paraphrased from Lord Baden Powell:
What you do speaks so loudly, they can’t hear what you have said.
Every veterinarian must learn to be an effective leader, especially when pursuing client-centered patient advocacy in well care. Every specialist must learn to be an effective leader, especially when developing satisfied referring veterinarians as well as satisfied clients. Every practice owner must learn to be an effective leader, especially when pursuing the team-based healthcare delivery model, and when leveraging a veterinarian’s time is important. In fact, every member of a practice healthcare team must learn to be an effective leader, for the sake of peers and clients, as well as the promotion of health for our patients.
Becoming an inspiring leader is not limited to one set of core values or leadership action-based taskings. Rather, inspiring leaders draw on a number of attributes and behaviors, all powered by their preferred emotional method. The choice is NOT whether you want to be an inspiring leader or not; it is a function of perceptions of the practice team and clients. My suggestion is that the 14 leadership skills I have published in many venues be combined with one of the behaviors or attributes listed above and infuse it into daily behavior with positive emotion toward the practice team and clients. Experience shows definitively that by doing so, a practice owner or manager will become perceived as a more inspirational leader and, in turn, have a more productive and profitable practice.
-----------------------
January 2015
The New Year- time for making those resolutions that will too often be forgotten by February. A survey of 1000 Australians found 69 per cent of us intend to make at least one New Year's resolution. And while less than a quarter of us will stick to achieving our goals, there is a secret to succeeding. A year-long study at the University of Hertfordshire in the UK found the key to keeping your resolutions varies according to your gender. For men, setting specific realistic goals, such as "lose five kilograms by April", rather than just "lose weight", is best.
Women should share their resolutions for the coming year with others, as, according to study leader Professor Richard Wiseman, "women benefit from the social support provided by friends and family". "If you halve your goal you'll be more likely to achieve it," dietitian Kate DiPrima says. "Instead of saying you'll exercise every day, make a commitment for three times a week. This way you'll have a sense of achievement rather than failure."
"The greatest danger in times of turbulence
is not the turbulence; it is to act with yesterday’s logic."
Peter Drucker, Management Guru
In a veterinary practice setting, it means looking at your written Standards of Care (SOC) and comparing them to the historical KPIs (e.g., key procedures per 100 transaction). It also means a time to assess the SOC document for long needed upgrades to the WHY and WHAT of that document. The WHO and HOW are protocols that belong to the staff, driven by the clear and concise written SOC document. WHEN is the time after the nursing staff has done the WHO and HOW protocols to meet with the key providers and establish time lines, success measures, and training commitment needs.
PLEASE - keep it real. Stating, "We will make 15% more money!" has nothing the staff can grab onto and work on to achieve. If you state, "We will book 10% more DG1+ dentistries each month, compared to same month last year.", that is something everyone can work toward. The RECOVERED PET and RECOVERED CLIENT PROGRAMS (10% more each month than the same month in the previous year) are also great goals for the front desk team.
So saying that about resolutions and resistance, I drafted the attached article to talk about change, transition, and the paradigms that prevent both. I hope it is helpful for the new year - and maybe, just maybe, a few of you will decide you need a savvy veterinary guide. My consulting programs are listed at www.drtomcat.com - also, unlike the newbies who "say" they are consultants, my philosophy is well established in the 15+ books I have published (most are available from Amazon.com, except the two new ones that are in the VIN Library for FREE download), and the 30+ monographs in the VIN Bookstore.
I wish you the very best in the new year, and hope your change transitions are exciting, fruitful and filled with wonderment.
Tom Cat >*-*<
Thomas E. Catanzaro, DVM, MHA, LFACHE
Diplomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
8 Sean Street
Boondall, QLD 4034
cell: +61 (0)4 1628 5975
Fax: +61 (0)7 3865 2368
Web: www.drtomcat.com
E-mail: DrTomCat@aol.com
Attachment: II IS NOT CHANGE
IT ISN’T CHANGE THAT DOES YOU IN – IT IS THE TRANSITIONS!
Thomas E. Catanzaro, DVM, MHA, LFACHE
Dipomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com
Faced with the choice between changing one’s mind/behavior
and proving that there is no need to change,
almost everyone gets busy on the proof.
John Kenneth Galbraith
It is not the changes that do you in, it’s the transitions. Change is not the same as transition. Change is situational: the new program, the new role, the new team, the new policy. Transition is the psychological process people go through to come to terms with the new situation. Change is external, transition is internal. The 3 P barrier (pride, process, paradigms) exists in most all veterinary practices.
Unless transition occurs, change will not take hold and flourish. That is what causes great ideas to fall flat. We have all heard the story, “The more things change, the more they stay the same.” Translating this syndrome into real practice-centered terms, “there can be any number of initiatives for change, but unless there are transitions, nothing will be different when the dust clears.”
Several of the important differences between change and transition are overlooked when people think of transition as simply gradual or unfinished change. When we talk about change, most people naturally focus on the expected outcome that the change will produce. If you are moving from California to New York City, the change may be seen as crossing the country (with multiple routes and key milestones), and probably learning your way around the Big Apple. The same is true for a veterinary practice changing to a team-based healthcare delivery format rather than a doctor-centered format, or maybe just establishing an electronic communication system for internal coordination between practice zones. In each case, the new arrangements must be understood if we are to be ready for the change.
Transition is different. The starting point for transition is not the outcome but rather, the ending that you will have to make to leave the old situation behind. Situational change hinges on the new thing, but psychological transition depends on letting go of the old reality and the old identity you had before the change took place. Nothing so undermines organizational change as the failure to think through who will have to let go of what when the change occurs. Transition starts with an ending!
To accept that transition starts with an ending is paradoxical at best! Test this fact with your own experience. Think of a big change in your life: your first veterinary practice position, or the birth of your first child, or a move to a new house. Good changes, all of them, but as transitions, each one started with an ending.
With your first veterinary practice, you had to let go of the student peer group and the safety of a bell curve assessment. You entered an arena where competency was required, and competency was excellence – mediocre (average) does not cut it in practice. With a new baby, you had to let go of a regular sleep, extra money, time alone with your spouse, and the spontaneity of going somewhere when the two you felt like it. Here too, your sense of competence may have been challenged when you found yourself unable to get the baby to eat or sleep, or even just stop crying. With a home move, a whole network of relationships ended. Even if you wanted to “keep in touch” it was never the same again. You used to know where to go for what: stores, the doctor, the dentist, the plumber, the neighbor who would house sit for you when you traveled. You have to let go of that feeling of “being at home” for a while.
Even in these “good” changes, there are transitions that begin with having to let go of something. There are endings. There are losses. The failure to identify and be ready for the endings and losses that change produces is the largest single problem that veterinary practices encounter in change management. This is the reason in consulting that we require NEW METRICS for new programs; if you do not change the measurements for success, you will most often revert to the old system that produces the old metrics.
I find practices that refuse to adopt the new spread sheets we provide, many of which are procedure specific, while the “old systems” used monetary metrics, which do not support a clear standards of care KPI per 100 transactions. We have a monthly budget projection, with paired income to expense center categories, but that often requires a realignment of the Chart of Accounts, which many practices resist. I have had some clients who would prefer to make excuses rather than accept a shortfall that exists in the old practice systems and concurrently they resist initiation of closure on outdated paradigms or the establishment of new metrics for new processes and outcomes.
Once you accept that transition begins with letting go of something, you have taken the first step in the task of transition management. The second step is understanding what comes after the “letting go”: the neutral zone. This is the no-man’s-land between old reality and the new. It is the limbo between the old sense of identity and the new. It is a time when the old way is gone and the new does not feel comfortable yet. It is for this reason that I modified our year-long consult to have quarterly revisits. In the early years, I made it optional, and those practice that wanted to “save money”, did not fund the quarterly visits; these practices had a high reversion rate. So I made the quarterly visits part of the year-long process, as well as a step-by-baby-step new training program to ensure staff developed into trusted team members, and our new program success rates increased. Sure, some practice owners wanted to short circuit the training process, and when they attempted that, the transition stopped and reversion usually followed.
It is important to understand the “neutral zone” for several reasons:
- If you do not expect it, and understand why it is there, you are likely to try to rush through it, and become discouraged when you cannot do so,
- You may mistakenly conclude that the confusion you feel is a sign that something is wrong with you.
- You may be frightened in the no-man’s-land and try to escape (some staff members take flight when faced with primary accountabilities), lending to higher than usual staff turnover as the programs are initiated.
- To abandon the transition situation is to abort change efforts, both personally and organizationally, and to jeopardize continuous quality improvement (CQI) initiatives throughout the practice team.
- If you escape prematurely from the “neutral zone”, you will not only compromise team member empowerment and change, but also lose a great opportunity.
- Painful through it often is, the neutral zone is the individual’s and practice’s best chance for creativity, individual renewal, and program development. The positive aspect of the neutral zone is realized after it is crossed, after the staff is trained to a level of trust, and after mutual respect becomes an operational reality.
The neutral zone is this both a dangerous and opportune place, and it is the very core of the transition process. It’s the place and time when the old habits are no longer adaptive to the situation, paradigms are challenged and many are extinguished, and new team-adapted programs begin to take place. It is the winter in which the old crops are plowed under and returned to the soil as decayed matter, while the New Year’s growth begins to stir and take root. It is the night where we disengage from yesterday’s concerns and start preparing for tomorrow’s opportunities. It is the chaos in which the old form dissolves and the new form emerges. It is the seedbed of the new beginning that most uncommon leaders seek.
ENDING – NEUTRAL ZONE - NEW BEGINNING
Most people make new beginnings only if they have first made an ending and spent some time in the neutral zone. Yet most practice owners try to start with the new beginning rather than finish with it. They pay virtually no attention to endings. They do not acknowledge the existence of the neutral zone, then wonder why their staff have so much difficulty with change.
I respect your misgivings, but concurrently, I don’t believe they represent real obstacles outside the leaders mind. I am not saying transition management is easy – only that it is essential. I have used the following change formula to defeat the old paradigm of A2 = G2 : If you Always do what you have Always done, you are going to Get what you have always Gotten.
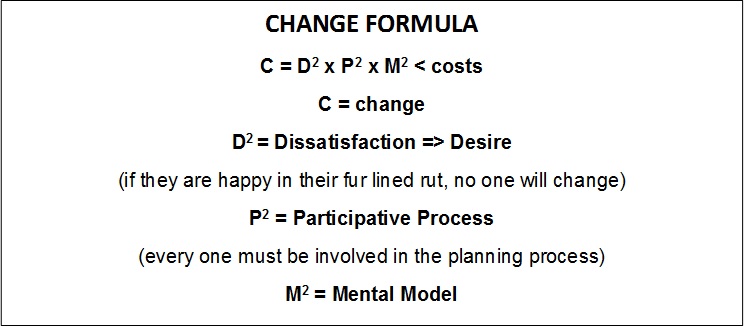
DR CAT’S CHANGE FORMULA:
Change – D2 x P2 x M2 < costs
D2 = discomfort => desire to change . . . if you are comfortable in your fur-lined rut, change will not occur until it becomes uncomfortable, which then drives a desire for change.
P2 = Participative Process . . . the power of many brains is part of the process, as is buy-in by the entire team, without team buy-in, change will not occur.
M2 = Mental Model . . . there has to be a clear methodology, including training to trust, to accept the new concept/model; people do not go into the neutral zone without some form of vision of where they are going.
Less than Costs = physical, mental, fiscal, social, personal, etc.
NOTE: primary factors are divided by multiplication signs, and if any one factor is ZERO, the outcome is NO CHANGE.
CAUTIONS!
- Please do not turn the whole thing over to individual contributors as a group and ask them to come up with a plan to change over to team-based programs. Involvement is fine, but it has to be carefully prepared and framed within realistic constraints; simply to turn over the power to people who don’t want a change (64% of the population) is to invite catastrophe.
- Please refrain from making change into small stages, combining first and second and then adding the third later, the change the managers to coordinators last. This one is tempting because in a process-oriented practice, small changes are easier to assimilate than big ones, yet one change after another is trouble and causes no relief from the original discomfort. It is better to introduce change on one coherent package.
- Please resist the temptation to pull the best people in the practice together as a model team to show everyone else how to do it. We know this is appealing, but it strips the best people out if the zones and hamstrings the zone team’s ability to duplicate the model team’s accomplishments.
- DO NOT SCRAP THE PLAN to find one that is less disruptive. Forget this option immediately – you had good reasons to initiate the change processes – it is your job as a leader to find out how to make it work!
- Do not tell people to stop dragging their feet or they will face disciplinary action. Don’t make threats, they build ill-will faster than they generate positive results – but ensure you have made outcome expectations crystal clear and concise.
So if you do not know how to get started, consider hiring a guide, a veterinary savvy consultant who understands the void of the neutral zone!