- Home
- About VCI
- Testimonials
- Contact Us
- Adventure CE
- VCI Programs
- VCI Ethical Values
- VCI Consultants
- Trusted Colleagues
- Initiatives to Watch
- Publications
- S@S Proceedings
- Design the Dream
- Veterinary Medicine & Practice
- Beyond the Successful Veterinary Practice
- Building the Successful Veterinary Practice, Volum
- Building the Successful Veterinary Practice, Volum
- Building the Successful Veterinary Practice, Volum
- Design Starter Kit for Veterinary Hospitals, 3rd E
- Healthcare of the Well Pet
- Promoting the Human-Animal Bond in Veterinary Prac
- Veterinary Management in Transition
- Veterinary Healthcare Services
- Veterinary Practice Management Secrets
- Newsletters
- Fortnightly Publications
- Fortnightly Articles
- Monographs
- Cat Sighting
- Pet Parent Sites
Veterinary Consulting International
(303)277-9800
www.drtomcat.com
|
Click below for the PDF's of the Fortnightly Articles or scroll down to read on current page:
November (mid-month) - Debate & Strategic Interactions October 2014 (EOM) - Zoning Concepts October 2014 (mid-month) - Patient Advocacy September (EOM) 2014 - Marty Becker Fear Free September (mid-month) 2014 - IQ vs EQ Leadership September 2014 - Program-based Budget Planning August 2014 - Family = HAB July (mid-month) 2014 - Beyond Problem Solving July 2014 - Veterinary Practice Images June 2014 - Multi-generational Team March - end of month- 2014 March - mid month 2014 End of January/Beginning of February 2014
September (mid-month) 2014
IQ vs EQ LEADERSHIP
Thomas E. Catanzaro, DVM, MHA, LFACHE
Diplomate, American College of Healthcare Executives
Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com
In his 1996 book, Emotional Intelligence, author Daniel Goleman suggested that EQ (or emotional intelligence quotient) might actually be more important than IQ. Why? Some psychologists believe that standard measures of intelligence (i.e. IQ scores) are too narrow and do not encompass the full range of human intelligence. Instead, they suggest, the ability to understand and express emotions can play an equal if not even more important role in how people fare in life.
What's the Difference Between IQ and EQ?
Let's start by defining the two terms in order to understand what they mean and how they differ. IQ, or intelligence quotient, is a number derived from a standardized intelligence test. On the original IQ tests, scores were calculated by dividing the individual's mental age by his or her chronological age and then multiplying that number by 100. So a child with a mental age of 15 and a chronological age of 10 would have an IQ of 150. Today, scores on most IQ tests are calculated by comparing the test taker's score to the scores of other people in the same age group.
EQ, on the other hand, is a measure of a person's level of emotional intelligence. This refers to a person's ability to perceive, control, evaluate, and express emotions. Researchers such as John Mayer and Peter Salovey as well as writers like Daniel Goleman have helped shine a light on emotional intelligence, making it a hot topic in areas ranging from business management to education.
Since the 1990s, emotional intelligence has made the journey from a semi-obscure concept found in academic journals to a popularly recognized term. Today, you can buy toys that claim to help boost a child's emotional intelligence or enroll your kids in social and emotional learning (SEL) programs designed to teach emotional intelligence skills. In some schools in the United States, social and emotional learning is even a curriculum requirement.
So Which One Is More Important?
The above example gives you some idea, and in many cases, veterinary school logic prevailed (‘A’ students will end up working for the ‘C’ students after graduation since “A” students have very little client rapport capability). From an academic point of view, IQ has been viewed as the primary determinant of success. People with high IQs were assumed to be destined for a life of accomplishment and achievement and researchers debated whether intelligence was the product of genes or the environment (the old nature versus nurture debate). However, some critics began to realize that not only was high intelligence no guarantee for success in life, it was also perhaps too narrow a concept to fully encompass the wide range of human abilities and knowledge.
IQ is still recognized as an important element of success, particularly when it comes to academic achievement. People with high IQs typically to do well in school, often earn more money, and tend to be healthier in general. But today experts recognize it is not the only determinate of life success. Instead, it is part of a complex array of influences that includes emotional intelligence among other things.
The concept of emotional intelligence has had a strong impact in a number of areas, including the business world. Many companies now mandate emotional intelligence training and utilize EQ tests as part of the hiring process. Research has found that individuals with strong leadership potential also tend to be more emotionally intelligent, suggesting that a high EQ is an important quality for business leaders and managers to have.
So you might be wondering, if emotional intelligence is so important, can it be taught or strengthened? According to one meta-analysis that looked at the results of social and emotional learning programs, the answer to that question is an unequivocal yes. The study found that approximately 50 percent of kids enrolled in SEL programs had better achievement scores and almost 40 percent showed improved grade-point-averages. These programs were also linked to lowered suspension rates, increased school attendance, and reduced disciplinary problems.
Observations
So what does it mean in a veterinary practice?
If you refer to the table above, you can see characteristics/traits of a successful leader on BOTH SIDES of the equation. The challenge is we select veterinary students based on IQ, and the years of school work hard at eliminating any EQ traits. EQ is client relations, EQ is staff empowerment, EQ is charisma! The journals are filled with IQ data points, as are our Association conferences and webinars. Contemplate this, what is more IQ than a webinar where you cannot read body language? Our downward spiral into IQ nirvana is becoming a slippery slope.
The charismatic veterinary leader makes mistakes and learns from them. Yet in veterinary schools, we increase the fear in students by 25% based an intimidation culture which has been present your eons. The fear of failure is ingrained in students before graduation, so learning from mistakes is NOT a cultural expectation in this profession. That makes incremental change scary but required. It also makes safe harborage for mundane factors like comparing Gross Turnover, the Average Client Transaction or expense percentages, three factors that have an UNKNOWN NET INCOME influence.
What would happen if a practice would compared lost clients to new clients each quarter? Where would the operational focus be shifted? An easier factor would be pharmacy income compared to pharmacy expense each month; yet most Australian practices still look at ‘Cost of Goods Sold’, which disguises line item comparisons such as pharmacy net income. Why would any logical person combine surgical supplies (zero mark-up), with nutritional supplies (30-35% mark-up), with pharmacy resale (~ 2x mark-up), with laboratory (50-100% mark-up), with DR Imaging (almost pure net), and consider it a rational comparison factor?
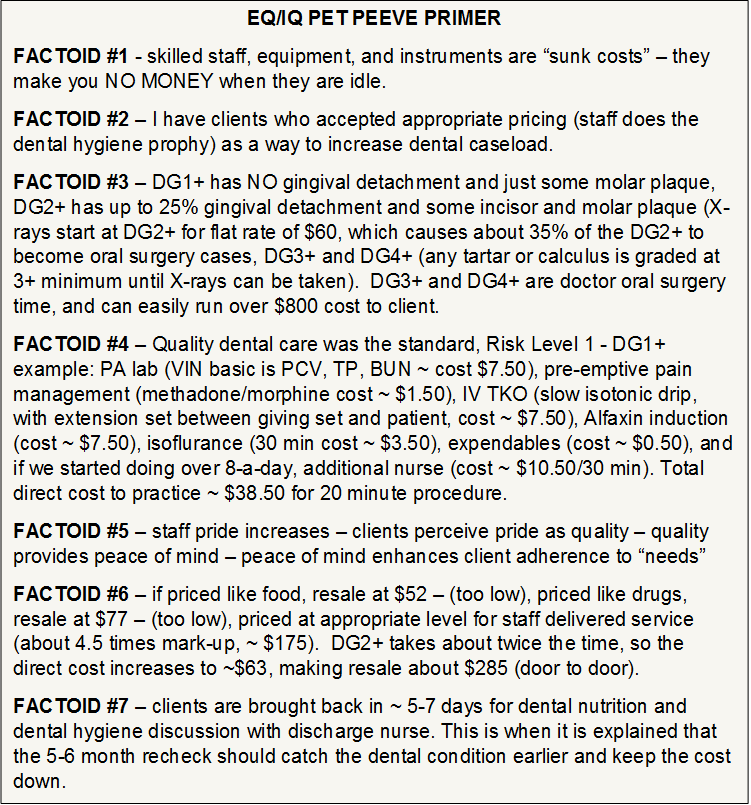
What would happen if a practice would compared dental cases booked to total patients seen during the month (dental specialists tell us 85% of adult animals have some dental need)? What would happen if a practice would compared nutritional referrals to veterinary nurses to number of patient seen (surveys show us that about 50% of adult animals have some prescription diet need)? All DG2+ mouths deserve dental X-rays, yet there are still veterinary practices without dental X-ray, or is they have one, are using it by exception. POINT – if the DR dental X-ray series is about $55-$60, regardless of number of images taken, and assuming they are taken by staff members, about 30-40% will become Oral Surgery (DG3+ and/or DG4+) . . . the secret is to keep the entry level dental care (DG1+ and DG2+) reasonably priced (i.e., appropriate pricing for staff delivered care).
Sure, our practice management software cannot give us this data easily. But why not? The basic business formula is “Income – Expense = Profit”, yet our veterinary software vendors say “sorry, can’t do that”, and we accept it. Why do we accept mediocrity?
Almost every practice owner and manager can give you the average expense % for common categories, but very few know the offsetting income center and/or expected profit margin for that line item. Think about it – Average is the best of the worst, or the worst of the best – it is the number in the middle – it is mediocrity.
This mediocrity continues into staff empowerment. Sure, most of us have seen dentists working with a 10-16 column per dentist appointment log, to allow for hygienist and whitening appointments. We have seen our physicians operating with medical assistants and nurses, with multi-consult rooms per physicians. And this year, the American Animal Hospital Association (AAHA) has declared 2014 to be the year for “team-based healthcare delivery”, yet I published the 500 page text with this title in 2008 and placed it in the VIN Library for free download.
THE PRACTICE SUCCESS PRESCRIPTION:
TEAM-BASED VETERINARY HEALTHCARE DELIVERY
//www.vin.com/Proceedings/Proceedings.plx?CID=TomCat2007&O=Generic
So, EQ is often right and IQ is often right. The reality is that the mix is needed. There are volumes now being written about mindfulness and happiness. These factors appear pro-EQ and contrary to IQ, but in the real world, it is all about team harmony and self-actualization (thank you Abe – Maslow that is).
You would think those with a high IQ would be looking for a savvy veterinary-specific consultant to facilitate their migration from yesterday to tomorrow, but it is the short-term thinking aspect of those with high IQs that often derails that engagement. I just came out of a practice that was floundering and stressed a year ago, yet after a year of consulting, they had harmony, liquidity and a 54% practice growth. Sure, that is an exception, but it is possible (e.g., 11 to 38% is the usual range of growth when the team is committed and the leader is willing to change)!
September 2014
PROGRAM-BASED BUDGET PLANNING
Thomas E. Catanzaro, DVM, MHA, LFACHE
Dipomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com About the time we can make the ends meet, somebody moves the ends. Herbert Hoover, 31st President Before we start, please understand, I don't see budgeting as an accountant's exercise. We publish a VCI Signature Series monograph, Fundamentals of Money Management, which differentiates between tax accounting and managerial accounting (it includes a Chart of Accounts diskette compatible with QuickBooks, by Intuit). I see program-based budgeting as activity and program planning for the coming year; it is a series of healthcare delivery commitments by the practice doctors and staff. The cash budget is only a series of clinical programs to which we have historical data on the income or expense impact on any practice. A good leader promotes income development activities and allows his/her team to increase net by controlling expenses and extending the healthcare delivery programs beyond the professional diagnostician. Therefore, the annual budget cycle includes, in my mind, the annual marketing plan and the communication/training plan for the team, as well as commitment to higher levels of quality healthcare delivery. PROGRAMS = NET INCOME More veterinary practice owners are learning that a focus on the front door is good business; they know when their procedures are down. A good program-based budget provides the needed measurements for growth; how many procedures are we doing, and what are the relationships to each other (e.g., dentistries to outpatients, fluids to surgeries, etc.). These measurements are essential to make success happen; it is also called have standards of excellence in the practice’s healthcare delivery habits. In the 1998 ISUP text, Building The Successful Veterinary Practice: Programs & Procedures (Volume 2), Chapter Four, and Appendices D, E and F, examples are provided that most any practice can follow to build a monthly cash budget, establish effective Income Statements, and build upon an established Chart of Accounts (the Chart of Accounts in Volume 2 expanded the AAHA system to include more income centers). Mechanically, the income statements of the practice should reflect the major income categories produced by the practice’s veterinary software at EOM, and those major categories are then used for the top left-hand column of the budget instead of "sales", and the income history of the last three years can be used to determine the average earning power of each month (percent of annual income). But the chart is not the planning process, and the planning and projections are what is needed to make it happen. CONTROLLING CASH FLOW The traditional approach to restrict expenses and inch the prices upward is adequate to maintain average growth to defend against inflation, but it does not promote expansion. The cost of professional services continually rises as do the fixed and variable costs. It is one thing to project an increased income for next year; it is far more difficult to cause it! The secret to obtain those extra degrees of expansion (practice growth) is based on the increasing horizontal (adding services) and vertical (expanding existing services) levels of income available to the practice. Income production (new or expanded services and products) is the major variable in controlling liquidity, also called "cash flow" by some. To control (or monitor) income levels, fees must be projected and cash must be received (and bad debt must be minimized). We will assume the practice has a clear set of values and core competencies, a future-based vision, and a CONSISTENT practice philosophy in place (an accepted core platform of services and products). This is started with a cash budget, with paired income and expense centers where possible, projected by month, for the coming fiscal year (see the 1998 ISUP text, Building The Successful Veterinary Practice: Programs & Procedures (Volume 2), Chapter 4, Program-based Budgeting):
Controlling the cash flow means knowing what is expected then measuring the accomplishment of that performance level. The program-based budget must be compared to actual performance on a monthly basis and adjustments need to be made in the remaining monthly targets if the year end goals are to be met; this is often done in dollars, but when variances occur, you must look at procedure counts or you are just fooling yourself. As I was surfing the net (AOL and NOAH), I watched veterinarians discuss their 1998 increase in gross, the percentage of gross which was due to vaccines or dentistry, and other such “first liar loses” type discussions. When are we going to learn? THE FRONT DOOR MUST SWING
The secret is what makes YOUR front door swing, Every practice has a different formula, but there are common components, and they are called programs (as in program-based budgeting). We realize that a pre-anesthetic laboratory screen is REQUIRED in virtually every case (although the intensity and scope varies), and as stated in a recent Nevada State Board letter, 80 percent of the surgery cases should have fluids running. (When was the last time you took a fluid therapy refresher for CE?). We have stressed the grades of dental conditions, and recording of the grades in the medical records, to the point where those doing it have doubled their income. We even have a Colorado practice who has contacted Dr. Marv Samuelson (VARL) for assistance to develop dermatology as an income center program (e.g., even in Colorado, 15 percent of the dogs coming in the front door have atopy). But let’s go forward with fundamentals and see what you are taking for granted, especially in surgical cases. We know in our hearts that pre-anesthetic blood screening is essential . . . one State Board has publically informed every practitioner in the State that 80 percent of surgery cases should be on fluids . . . we read about pain management, and listen to seminars, yet believe clients can make a knowledgeable decision about pain management with no training - post-surgical pain killers are not optional - everyone knows PAIN IS INHUMANE! Yet every day, there are practitioners putting animals at risk, and themselves into liability, by practicing wallet medicine instead of quality medicine. How about radiology? Fact: most every practice has forgotten that a radiographic baseline of the thorax is good medicine. A boarder who is coughing does not always have kennel cough. Dogs do have other problems. For instance, a negative Difil test tells you about circulating microfilaria, not adult heartworms in the thorax. Current literature shows that some of the coughing cats previously diagnosed as asthmatic are actually heartworm infested, even in non-endemic areas. ONLY an X-ray can do this effectively. Consider this: Dr. Bob Smith (radiologist, University of California - Davis) believes that dogs with a negative OR positive heartworm test still deserve a thoracic X-ray series before starting the preventive care or treatment protocol. Moving on to the abdomen, when was the last time you did an IVP or cystogram? There are more things than just foreign bodies occurring in the abdomen. Have you ever considered the diagnostic advantage of a Baro-spheres when doing a laparotomies, since leakage is not a by-product of these pellets? During a short course recently held, it was stated, “Use of the Penn Hip technique to aid in the diagnosis of hip dysplasia and the introduction of Baro-spheres for barium studies have proven diagnostic advantages”, and one of our clients attended and KNEW he could go back to practice and virtually double their income in this area. Look at the advances in cardiac evaluation. The handheld ECG which gives a lead-II rhythm strip can be used with every annual life-cycle consultation (yes, I know you call it an annual exam, but which sounds more accurate?). The handheld ECG is economical enough that if it was used for each “annual”, at a fee of $2.00 additional, it would be totally paid for in less than six months; then it is a NET-NET program every time it is used! The use of echocardiology is on the rise; within five years most quality practices will be using it regularly. This modality is technique-driven and relatively easy to read; the difficulty lies in determining where and how to place the transducer. As Dr. Larry Tilley states so often, “Telemedicine now allows a practice to be in contact with a specialist - even across the country - within minutes”. Reflect on the blood pressure diagnostics of your practice. It cannot be emphasized enough. Every practice should be using a blood pressure device daily (e.g., Doppler). We have some practices which ensure that the feline blood pressure monitoring is part of the annual life cycle consultation. It has been shown that 60-plus percent of the cats in renal failure can have hypertension. It has also been shown that hypertension can be manifested in such unusual signs as anisocoria. Dr. Mike Garvey (AMC, NY) has stated that blood pressure measurement is paramount - for more than hypertension . . . up to 30 animals die every day from hypotension for every animal that dies from hypertension. ECONOMICS 101 ALA DR. TOM CAT “Tom Cat, we will damage our relationship if we add these unneeded diagnostics.” You are right, if they are unneeded. But in every case stated above, there was a medical need. The fact that you have taken radiology for granted means the overhead is still larger than the income from the program center. Yes, program center -- not income center, not profit center. The front door swings because we believe in our health care programs and share that conviction with clients as NEEDS for their animal(s). If you don’t medically believe it is needed, NEVER do it! And for those of you who take one film to “save the client money”, remember what every text and radiologist has stated, “If it looks like a duck, sounds like a duck, and walks like a duck, it must be considered a duck . . . and ducks state very clearly, QUACK, QUACK, QUACK!” If radiology is needed, two views are needed. To provide half the care is a violation of professional ethics and the Practice Act. Think of lameness cases where you have said, “If this does not get better, we may need to take radiographs”. The client brought a suffering animal to you because they wanted “PEACE OF MIND”, and you only offered them “tincture of time”. And you wonder why they never come back? Lameness generally requires radiology to determine the appropriate treatment as well as the prognosis, and in client relations, they came to you because you are the diagnostician! The ability to believe in good medicine is the cornerstone of a successful practice. The ability to convey this need to clients is the cornerstone of a profitable practice. The overhead of a veterinary practice is pretty fixed (in well managed practices, less than 50 percent of the gross income is spent on monthly P&L expenses, not counting rent, doctor monies, and ROI benefits (quarterly rate stays below 48%). So, it is the delivery of services and products within existing staff and facility capabilities which can make the net income difference. TODAY IS THE FIRST DAY OF THE REST OF YOUR LIFE We really don’t care what you have already done; that is past. What we care about is what you are willing to do. Every year, new continuing education courses mean you have the opportunity to enhance practice programs. The continuing education experience which does not add one new program per day of CE attended was a wasted expense. The new program is designed to provide better care, and there is a value associated with that client benefit. That value, as assessed to clients, should be reflected in your program-based budget for the year. The cash flow reports from that computer in your office ONLY reflect the “belief level” of the providers in the new program(s) being offered. The choice is yours, we are here to help, but the belief starts in your gut and ascends to your heart. When your heart believes in the program, the clients will accept the care as needed and essential. It is your choice -- lower the net each year, or provide better health care delivery programs.
JUST DO IT!
THE PRACTICE BUDGET TEAM The control of the cash flow from programs that match the core values of the practice is a team responsibility and as such, the plan must be a team effort. The practice budget team should include the practice owners, bookkeeper, office manager, lead technician, lead receptionists, and an outside mentor. The technician and receptionist should be involved in those areas where they have a first-hand interest and impact but need not be involved in all parts of the team planning. The outside mentor can be a CPA, consultant, attorney, or psychologist. To be most effective, they must be detached from the practice's patient healthcare plan. To be most effective, this entire day of isolated planning sessions is without spouses. The spouse, as with any client, usually has a hidden agenda and will muddy the team effort, even if just to wait on the sidelines for a meal companion. It would be appropriate to form focus groups of respected clients to discuss potential healthcare service opportunities before the off-site planning session. After the budget planning session, this type of client-centered input may be counter-productive to the success of the plan. The budget planning team needs a playing field (established rules and historical game experience), and that is usually the past financial statements. The planning team needs to meet at an off-site location about three to six months before the fiscal year begins and use the historical data to develop a strategic plan for the practice's cash flow. To be most effective, the practice manager becomes the meeting coordinator and handles all the following:
a) For the key team members (owners, practice manager, and CPA or bookkeeper), possibly with a mentor, start at 7:33 a.m. with a very light breakfast (the mind works better on a lightly filled stomach), coffee, tea, and juice.
b) At 7:57 a.m., start review of the previous financial statements using an overhead projector so all can see and discuss the key elements (view graphs prepared of previous fiscal year, all twelve months, of the income statements and balance sheets).
c) Have a practice cash budget outline prepared using percentages per month per element of income or expense, as available, for handout after the historical review and before brunch.
d) With the arrival of the adjunct team members (associate doctors, lead receptionist, and senior technician), provide a light brunch at 10:37 a.m. e) With the expanded planning team, start a review at 10:56 a.m. of the projected program-based budget percentages that were developed from historical data on the previous practice team performance and client utilization habits, and brainstorm which programs can be added or expanded in the next fiscal year (don't kill a single idea during this brainstorm, just write them down and tape them to the wall).
f) At 12:30 p.m., break for lunch on-site, resume at 2:04 p.m. to develop expected income per program area of interest to support cash budget. This is often where the "reality check" is provided by the nurse technician and client relations receptionist to mediate the "grand ideas" of the key team. Human resources are only so flexible and expandable, and these two persons must stand up for the quality of life of the staff. Pros and cons, alternatives, and methods to reach the "grand ideas" need to be the target of the discussion, but it may require adjusting the personnel budget, equipment budget, or even the facility size.
g) Soda, juice, coffee, and tea break at 3:31 p.m. Key staff rejoin at 3:47 p.m., but without CPA/bookkeeper, technical assistants, and receptionist (released for remainder of day).
h) Resume with emphasis on new business areas, marketing potentials, and client acceptance factors. Extra expenses (e.g., training, space, equipment) to support new income areas need to be explored in detail. Compromises will now be required based on the input provided by the lead nurse technician and receptionist coordinator. At least 60 percent of their ideas need to be incorporated to have the budget be perceived by the team as realistic and a useful process.
i) Supper break at 5:45 p.m. for two hours, time to relax and unwind. Attempt to stay away from excessive food or drink indulgences, since there is still work to do.
j) Rejoin at 7:46 p.m. for a "wrap and polish" session of all that has gone before, to expand on core competencies, core values, and practice philosophy applications. Ensure you include a staff impact assessment and communication plan. This may include an additional training budget. Also center on those portions which were provided by the technician and receptionist that could not be used, as well as the changes that will be needed to make the annual program a success. The need for the communication plan is critical for two elements: the paraprofessional staff and the clients. A draft transition plan, a month-by-month sequence of changes or additions for the next year, would be an appropriate and organized method to communicate the decisions of the budget planning process. This plan should integrate all the different plans, and ensure that no member of the staff would be tasked with more than three new functions/habit changes per month.
MINIMUM BUDGET DISCUSSION ELEMENTS
The syllabus and the refined agenda discussed above need to contain certain elements, including: equipment, debt retirement, quarterly financial comparisons, cash outflow discussions, receivables, bad debt allowance (less than 1.5 percent), charity at the exam table (less than 3 percent of gross), employee discounts (less than 20 percent without IRS complications), tax laws, space potentials, computerization upgrades, people allocation per area (based on gross, with quarterly targets, such as 8.5 percent technicians, 7 percent receptionists, 2 percent kennel, 3 percent administrator), and finish with a fee schedule that supports the budget for people and equipment upgrades. Key financial and operational relationships need to be discussed, to determine indicators that management can observe to easily monitor trends on a monthly basis. Examples would include, but should not be limited to:
Some ratios, like the "Pharmacy Sales to Diagnostic Sales" by veterinarian, is a very individual ratio, but centers the doctor's attention on what they can do for the quality of care provided by the practice. Many of these can be graphed for more clarity when evaluating trends. In the ISUP text, Building The Successful Veterinary Practice: Programs & Procedures (Volume 2), there are eleven graphs and two charts in the Appendix for watching “the tips of the practice iceberg” on a monthly basis - we call it a dozen dots a month, although it is a baker’s dozen (13)! These are indicators to watch so you know when to look deeper into the operational trends or fiscal management of the practice.
Beware of the easy factors so often published without "the rest of the story", such as average client dollars per transaction (ACT). The ACT is often counter-productive since it centers attention on the wrong thing. What is the "computer's definition" of a transaction; is the ACT reported by veterinarian or by hospital; what is the over-the-counter sales impact; what is the income per inpatient visit versus outpatient visit; what are the payroll hours per transaction; what is the return rate per year (client or patient)? Some consultants demand that the square footage of the practice be used to compute cost centers, but the allocations of circulating space makes potentially profitable areas appear worthless. Evaluate services within the resources available to the practice and maximize income from each cost center. The bottom line of fee structuring is simply, if you are within about 10 percent of the community high, variances from national norms are not significant for the clients who seek quality veterinary healthcare services! The veterinary computer systems of today are designed to give abundant "data". This most often is minimal "information" for management decision making. A savvy practice manager must be able to take the information available and process it into knowledge that can be used for the good of the practice. In any practice, less than 30 factors are needed to reveal the monthly trends. In the area of laboratory services, expenses should be tracked by in-house versus commercial and income should be tracked by preventative, pre-surgical, and medical support functions. The examination/office call (better called "doctor's consultation") should be tracked by rechecks, normal, and extended consultations. In a healthy, mature practice, monthly operational expenses, without the major variables of rent, DVM salaries or return on investment (ROI), would be expected to be between 45 percent to 48 percent of the gross. The AAHA Chart of Accounts, expanded in the ISUP text, Building The Successful Veterinary Practice: Programs & Procedures (Volume 2), provides an easy access and comparison to the regionalized database of the profession. Quicken or QuickBooks (from Intuit) are excellent software systems for expense summaries and accounts payable needed to support the Chart of Accounts. Comparisons could include: outpatient drugs and medical supplies versus inpatient drugs and medical supplies, vaccination income as a percentage of gross, hospitalization income, X-ray income compared to expenses, over-the-counter sales, nutritional sales of prescription versus other products, boarding fill rate, baths per transaction, or the eleven fiscal charts provided by Catanzaro & Associates, Inc. Other expected ratios include rent at one percent per month of the fair market value (triple net lease), DVM wages (owner(s), et al) at 18-23 percent, CPA and legal fees at 0.8-2 percent, office supplies at 1.4-2.2 percent, or maintenance costs of 0.5-1.5 percent. In more progressive practices, healthcare parameters such as ECGs per thoracic X-ray or kidney dysfunction laboratory profiles per six-years-old or older canines examined are monitored since they relate to income potentials. MANAGERIAL EFFORTS Using the practice team to keep the budget plan on track will be enhanced when the accurate data is shared in a timely manner, using a format that is user friendly. Remember, the staff knows how much a practice takes in each day (they close out the computer), they just don't know what the costs are in most cases. The team which is used to keep the budget on track will provide feedback which will show the benefit of the time taken to make the information readable. The practice management methodologies required to make the budget plan happen is as simple as driving "A TRUCK", or in easier terms:
A = accuracy of data
T = timeliness of data availability
R = reformatted as information
U = user friendly
C = control cost of capturing data
K = keep on track monthly
The use of a posted "Dinner Bell Chart" (Building The Successful Veterinary Practice: Programs & Procedures (Volume II), Appendix), helps the staff see the monthly income participation. It is simply a graph with appointment days on the horizontal axis and income on the vertical axis. The target line (done in highlighter) starts each month at zero and ends at the cash budget projection for that specific month. The daily gross receipts are posted on the chart at the end of each day, in a cumulative fashion ($1860 on day one, then $1435 on day two, would put the day two dot at $3295). The gross income dots are connected in dark ink each day. At the end of the month, if the dark line is above the highlighter line, the owners take the staff to dinner. While at dinner, the dinner site of the next Dinner Bell Chart celebration is chosen by the staff. If the cost of the site selected seems excessive, the owner simply adds that to the target before announcing the cash projection figure for the next month. As an added benefit and team builder, each third Dinner Bell success celebration should include the families or significant others of the staff members. They make the practice success sacrifices, too. When the staff centers on offering the services each animal needs (or the practice needs for professional healthcare decisions), the income should take care of itself. This statement is based on four assumptions:
1) that caring practices only "sell" peace of mind -- they give the client two "yes" alternatives which they are "allowed to buy" to meet the needs stated;
2) that the veterinary practice environment for horizontal and vertical diversification has been developed;
3) that it is well understood by the staff and healthcare providers; and
4) the team has been appropriately trained in both competencies required and client communication techniques.
These four assumptions are easier said than done, but that is the art of management rather than the science of accounting. The program-based budget is a system based on quality care, client-centered service, and patient advocacy . . . the accountant’s propensity for stating the obvious with an expense-based budget must be left in the past as lessons learned . . . the future is in making the front door swing, more times for your existing clients.
August 2014
FAMILY = PET BOND = PROFIT
Thomas E. Catanzaro, DVM, MHA, LFACHE
Dipomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com
HAB = human animal bond = the interaction of people and animals in our society = profit center of the future.
A majority of veterinarians make their living because of the human-animal bond, yet most veterinary practices do not capitalize upon the potentials available. The client calls the veterinarian because they have a concern about the well being of their animal and want an expert to assist them during their stressful decision time; they want peace of mind. The basic premise which needs to be taken when the phone rings is that “the phone shopper” wants a quality-based, caring veterinarian at “an affordable value”. A phone “emergency case” wants to be told they have done the right thing by calling and should come into the practice. No client who calls wants to be told to stay home.
The contemporary pet programs such as active pet selection assistance (AVMA©), pets by prescription and the Pet Partners© certification program (Delta Society©), Prescribe Pets Not Pills (VPI Skeeter Foundation©), and behavior management (AAHA©) promote the human-animal bond while supporting the healthcare reverence for life and quality of care programs. Many Veterinary Teaching Hospitals are starting telephone “hot lines” for pet owners to allow the students who volunteer to better understand the stress of animal stewardship grief and stress. A multi-faceted, interdisciplinary group, sponsored mainly by Hills, named VetOne©, started publicizing the family-pet-veterinary bond at major veterinary meetings and in our media as we entered the new millennium. The text, Promoting the Human-Animal Bond in Veterinary Practice, was released in May 2001, and the second edition was published by the VIN Press in 2009 with a new well care chapter; it has 26 appendices of practical application programs. HAB information abounds, but practice commitments vary.
Definition of BIOETHICS: applied ethics to real-life, day-to-day problems of ethical decision making in health care delivery.
In the past, veterinary ethics have been forensic (legal) values we used to describe the professional approach to veterinary practice, but bioethics are the values we use personally in practice. Sometimes the veterinarian is the person who makes the bioethical decision, sometimes it is the person answering the phone, and on some occasions, it is the person who observes the suffering inpatient in a cage. But more often, the decision is laid at the feet of the lay people we come into contact with -- family, clients, public officials, judges, humane societies, and others. There is seldom any clear bioethical solution. Rather, there needs to be an awareness of its existence within the veterinary practice environment.
CHOOSING A THERAPY WHEN DOCTORS DISAGREE
This situation presents a wide array of ethical issues. Whether or not the client should be informed of the nature and prognosis of the illness is certainly pertinent, but is hardly the most significant question in the bioethics at hand. Attention should be focused upon a cluster of three basic ethical questions raised in this case:
The option to be chosen in each of the above three questions is not just a medical decision based on scientific training, but rather, a professional value judgment. When a healthcare team is being developed, these cases deserve a full staff discussion so the professional logic, subjective feelings, and practice core values become established so others can make similar decisions in the future.
ACTIVE EUTHANASIA
The American Medical Association states that active euthanasia is illegal, but they only deal with one species of animal. Exactly what are the fundamental measures of animal value and worth which require the veterinary bioethics to be evaluated?
The alternatives in euthanasia are generally not based in veterinary science. They are based in personal value systems and practice philosophies. In many of the practices we support, we suggest a “pain” versus “suffering” discussion when the patient is entering the golden years, when there is malignant oncology present, or other debilitating or chronic syndromes. Be proud that we can treat pain in many ways now; many clients do not know this. Suffering on the other hand, is often a subjective value observed by the client, including the animal soiling its den (urinating or defecating uncontrollably at home), bumping into walls due to poor eyesight, inability to maneuvering stairs, snapping at the children when startled due to loss of hearing, or similar behavior challenges. We spend the extra client time ensuring they know that we can “treat pain”, so they need to call whenever it seems to be present, while in a case of “suffering”, the client must tell us when the love of the animal outweighs the loss of the companion, and it is time for euthanasia.
ANIMAL ABUSE OR NEGLECT
This issue is sad but raises no difficult questions of principle at all. If there is a violation of the Animal Welfare Act - Code of Federal Regulations (CFR), Title 9, Chapter 1, Subchapter A, there is neglect; if the act was intentional, it is usually considered abuse. Presumably in these cases, the individual or the family who has support responsibilities for the animal(s) is deemed inappropriate to the animal's welfare. But the veterinary practice which makes the decision to elevate the issue to the authorities must face bioethical issues.
When a practice promotes behavior management services, starting with house training, the incidence of neglect decreases in the clientele. Most clients are unaware of proper animal care, since they learned from their parents, who in many cases either came from the farm, or had parents who came from rural America, where farm dogs and barn cats had to fend for themselves. Like parenting, there are very few prerequisites in our family stewardship system, so if we do not do it in the veterinary practice setting, no one will. This is a wonderful area for staff bonding with clients, and the brochures and literature from AAHA make a great starting point, along with the appendices of the above mention text, Promoting the Human-Animal Bond in Veterinary Practice.
THE KEY QUESTIONS
It is often said that issues of bioethics fall into two categories: some concern procedures for decisions, others the substance for decisions. The distinction, while intuitive, is not easy to sustain. How do we know which values should be followed unless we know what values should to be sought?
In biomedical ethics, there are usually five basic decision-making agents that require consideration by the veterinary practice:
There is a traditional adage in medicine, that is, "First, do no harm". In the previous bioethical issues, some would feel that the solutions were clear and definitive, that ethical issues do not exist. The areas discussed are illustrative of veterinary medical situations where there is room for reasonable people to disagree. The reason for this discussion was to make the concept of ethics in biomedical decisions become a reality, to show that bioethics do apply to veterinary practices, and to offer the opinion that bioethics should be an element of the decision making process in quality health care delivery in the veterinary practice.
THE PSYCHOLOGICAL BOND
The American Veterinary Medical Association developed and has available all the documents and aides needed for active pet selection assistance by veterinary practices, including some very well done color brochures. The AVMA also introduced the Lost Pet Kit over a decade ago, yet many practices have neglected to integrate it into their practice programs; with digital photography, it is easy and takes very little space! The Delta Society has developed the protocols for Pet Partners and pets by prescription within the community and school environment. Either of these programs can develop new pet owners, clients who are already bonded to the practice since they selected their pet with the expert assistance of the veterinary professionals of that facility.
Human-animal bond resources are available at almost no cost to the veterinary healthcare facility. There are multiple human/companion animal bond (H/CAB) programs available from associations and other non-profit organizations, and 26 are listed in the appendices of Promoting the Human-Animal Bond in Veterinary Practice. The international clearing house for interdisciplinary HAB groups and programs is the Delta Society (800-869-6898). The American Veterinary Medical Association (708/925-8070) has the pet placement handouts and information as well as hosting the American Association of Human Animal Bond Veterinarians (AAHABV – which has a very small membership fee).
The best companion animal practices realize they "sell" only one thing: peace of mind for the client. They concurrently are a patient advocate and tell the client what is needed for the best of the pet, either of wellness or professional diagnostic concerns. The client is allowed to select from the list, they are allowed to "buy" what they think they can afford. Lesser cost alternatives are not offered UNTIL the client asks for lesser cost alternatives, but the "options" must be kept in perspective of lesser diagnostics, lesser response rates, or lesser probability of desired healthcare effects. Clients prefer to "buy" and hate being "sold" in most every occurrence, and a smart practice leader trains and rehearses the practice team to "sell" ONLY peace of mind, freedom from fears, or psychological comfort while allowing the client to "buy" products and services to their heart's content.
Dentistry is a common human-animal bond practice program . . . lack of oral hygiene is a cause of breaking the human-animal bond, as in so bad a breath that it would choke a horse. Restoring “puppy kisses” is the ultimate benefit of a dental prophy, but is seldom mentioned. When a practice starts to “grade” teeth, magic happens, especially with differential pricing. Dentistry is becoming a quotable commodity, so pricing is a community positioning action as well as client bonding action. The Holstrom, Frost Eisner dental text makes a clear differentiation between Tartar and Calculus, which I use here:
DISCLAIMER - in some areas of the USA, the above example prices are only 50% of the going rates. We usually recommend to phone or e-mail clients, where we have not assessed the community, that veterinary practices with a single dental rate peg their prices by using their current fee as the 2+ prophy rate, decrease by 25-33% for the grade 1+ prophy, increase by 50-75% for the 3+ oral surgery fee, and at least double for the 4+ oral surgery.
Behavior management is one form of HAB practice service; it is one of the hottest topics on the continuing education seminar circuit in recent years. A survey of Internet searches shows behavior management is the #2 reason for new clients selecting a practice (location was #1).
The primary problem is proactive behavior management services are a staff function as much as a professional service, and the staff members seldom get to attend the seminars. Obedience training is not behavior management, it is most often handler and location specific. HAB behavior management is teaching and rewarding the pet an appropriate family behavior by positive reinforcement. Allowing the client to "buy" these services is a client privilege most practices do not yet offer. Behavior management programs are easily initiated for dogs using the Gentle Leader head collar (usually provides “power steering” in less than 8 minutes when you understand that “release of pressure” is the animal’s reward of that device). The 65-page head collar booklet provides the techniques needed for behavior management, but the "caring" practice offers their nursing staff as “head collar fitters” at sale, and as trainers to help the client if they get stuck ($20 per appointment). This veterinary practice behavior management effort often leads to Puppy Clubs, Kitten Carrier Classes, Senior Clubs, and other client "social" programs (e.g., Guinea Pig Pig Out) which add to the practice bonding (and concurrently increases the client return rates -- and practice liquidity). In some cases, the practice supports a Pet Partner Program (Delta Society), and gains from the community good will and human interest media stories.
Behavior management is a potential practice area for staff to excel. Most are client education programs best done by trained staff members (e.g., house training, feeding, new owner orientation classes, etc.). In America, over 6 million animals a year lose their home and often their lives because of behavior problems. It is worse in many other countries. The veterinary practice team which helps prevent this "disposable pet" syndrome not only keeps clients, but gains positive recognition in the community. Recognition for helping animals is a marketing benefit to the practice without having to advertise or market routine services or products.
Nutrition is the ultimate human-animal bond for most clients. Clients like to feed their pet, because it makes the pet seem happy. We know that premium diets and quality nutrition will extend the active life of most companion animals, but we often forget to tell clients about “smaller stools” or “better smelling cat boxes” when feeding the highly digestible premium foods. Prescription diets should be treated like any other prescription, and be actively monitored by the paraprofessional staff at 2 to 4 week intervals; these can be “no cost” courtesy visits with the “nursing staff”, since purchase of goods usually accompanies a visit to the practice.
Changing “boarding” to a Pet Resort, or Canine and Kitty Camp, and changing “kennel kid” to animal caretaker, can change the atmosphere of the separation encounter. Using a Kong Toy for “yappie hour” (if they purchase a Kong Toy at guest check-in, a special feeding using the inside of the Kong Toy will be done at 5 p.m. daily, like a happy hour). When the pet goes home with the Kong Toy and “yappie hour” habit, when the client comes home from work and is greeted by a leaping bundle of fur, they can provide the Kong filled with food, and get changed into their doggy play clothes while the pet is occupied (P.S., Kong Toys are dishwasher safe, and almost indestructible, while not looking like anything in the home, except maybe the Michelin Man).
THE BOTTOM LINE
As a full time consultant, what I miss most about practice is “puppy breath”. Like most all veterinarians, our staff joins veterinary medicine because it is a “calling”; we know they do not join for the meager salary and benefits alone. When we can promote hospital staff as patient advocates, human-animal bond specialists, and “nursing” staff (a term the clients understand very well), we can reinforce the “warm fuzzy” aspects of this rewarding profession in their hearts and minds.
In a recessionary economy, clients stay home more, see their pet more, and will strive to fulfill “needs” while they postpone “wants”. Since 9-11-01, followed by the GFC (global financial crisis), practices which had been using the word “need” for healthcare have had greater client access; after 9-11, most had the best October and November in their history. Practices that clung to the nondescript “recommend”, or those that offer multiple options and expect client expertise to make rational decisions, had slower months than ever before; clients do not want to make choices when stressed, they want to be told what is needed by someone they trust.
Explore every client contact for those moments when the family-pet bond can be promoted. Listen to the Dr. Marty Becker “fear free” initiative being copied at many levels; brainstorm the concept with your staff to get real excitement going. Use every opportunity to acknowledge the important role the companion animal plays by providing their non-judgmental love in these times of stress and worry. Allow the practice staff members to select HAB areas of interest, help them develop a working knowledge of the subject material and healthcare delivery options, get them practice business cards with their new title (e.g., pain management advisor, veterinary dental hygienist, behavior counselor, nutritional advisor, etc.), and start to promote their interest and new knowledge as a client benefit. Celebrate the bond every day in every way!
July (mid-month) 2014
BEYOND PROBLEM SOLVING
Thomas E. Catanzaro, DVM, MHA, LFACHE
Dipomate, American College of Healthcare Executives
CEO, Veterinary Consulting International
DrTomCat@aol.com; www.drtomcat.com
Obstacles - those frightful things we see when we take our eyes off our goals. T.E. Catanzaro, DVM, MHA, LFACHE
Some practitioners erroneously believe that solving immediate practice management problems is the best way to change productivity and performance. A better approach is to cultivate ideas whose application and impact range beyond the task of the moment. Overcoming inertia and getting things done rely on follow-through and breakthrough skills. BREAKTHROUGH SKILLS
As a team leader or a team member, you must first learn how to present your ideas in a comprehensive and enlightening manner: * COVER YOUR BASES. Before you show off your personal planning skills, make sure you are seen as doing a good job with your current responsibilities. If you don't have time to think beyond the immediate concerns on most practice days, delegate the more repetitive day-to-day responsibilities to dependable staff members. * NETWORK. Before you suggest an idea at a team meeting, try to get a feel for the other team members' interests and concerns. Know the problems they face and the solutions they have developed and address the issue at hand in terms that include their interests. * SEEK OPPORTUNITIES. View problems as opportunities to solve challenges. A strategic thinker sees multiple alternatives in events that others view as crises or failures. Nurture this attitude within the practice team.
* BE POSITIVE. Make your suggestions in a non-confrontational way. If your idea impacts others, soften your approach with phrases like "What are your thoughts on . . . ?" Remember, the staff within most every practice cares, they want to help, and their suggestions most always come with good intentions. Look for the caring intention BEFORE you evaluate the idea(s). * DON'T LIMIT YOURSELF. Do not hesitate to make suggestions that are not related to the bottom line. Clients must believe you care BEFORE they believe in your health care plan. The value of an idea to a practice is measured in quality of life as well as quality of care. Practice benefits can and should go beyond the cost-saving or profit-producing ideas.
FOLLOW THROUGH SKILLS Planning a project can be completely different from its implementation and far more difficult than ever anticipated. When projects stall, everyone becomes frustrated. Projects stall for many reasons, but the obstacles which initiate the stalling have some commonality. The first secret to proactively enhance the follow through is to recognize obstacles of your own making: * FANTASIES. The mind can envision how well a plan will work, and it is far happier than when overseeing the actual implementation hassles. You need to set the fantasy aside and get your hands dirty. Edison had a vision of how a light bulb should work but had to build over 1,000 of them to turn his vision into reality. Are you ready for 999 failures to become famous for your new ideas within the professional or client-based community? * FEAR OF FAILURE. Fear that results will fall short often cause us to let a project quietly die rather than live with poor results. Remind yourself that concrete results, even those that fall short of expectations, are far better than none at all. * INVISIBLE RUTS. A common pitfall is mindlessly following old habit patterns. We have learned from what went before, and know what works, but the practice plateau or lifestyle stagnation is caused by "non-change" rather than the pursuit of unique or new experiences. Ask if those old stale protocols are important and determine "why" if the tendency is to retain them. If the "why" is simply, "We have always done it this way," then bypass them, as necessary, to get things done. * COMFORTING MYTHOLOGIES. Don't fall prey to the slogans or comforts of tradition. Southern California community needs are different than the rest of the USA, suburban needs are different than small town rural America. Marketing gimmicks must be tailored to the community needs, not to the practice by some article or consultant who has not even been in your practice. If you believe "everything is fine as long as everybody is busy,” you might overlook the benefits of new projects. * EGOTISM. Thinking that your own intuition and insights are infallible cuts you off from your colleagues' ideas. Doctor, paraprofessional, or animal caretaker, it does not matter. Everyone has a mind and each mind has unique ideas to share, if harvested in a caring manner. Objectively review all suggestions, including your own, and implement the best. * FAILURE TO DELEGATE. You may be shouldering the whole burden because nobody else is as effective as you are . . . or because you don't want to share the credit when a project is done. Either way, you place the project at risk. Your odds of success increase greatly when you take on only the tasks that suit your abilities best and let others take on the rest. Train each person to a level of trust, then delegate the accountability for the outcome to them (not just the process). Let them improve the program(s). * INFLEXIBILITY. When an approach is not working, substitute something more positive. If your staff does not implement your ideas, ask them for alternatives. Let them develop unilateral plans and put those into action, then evaluate at 90 days for benefits. Never veto ideas just because they are not yours! Flexibility often requires taking a step backward, but ends up being more productive. * LOVE THE INTRIGUE. They are either with you or against you, right? Put aside petty intrigues and enlist everyone's help. A "them versus us" practice staff will never be a health care team. Only "we" can cause harmony and success. If you love intrigue more than progress, or you prefer to take credit and give blame rather than take blame and give credit, go into politics or the spy business.
POWER UP FOR PROBLEM SOLVING In our daily routine of practice we rely upon habits to get the job done, but when we need a creative or innovative solution, many veterinarians don't know where to start. There are tools that teach creative problem solving. They don't give you genius, they simply pull out the genius within you. For those practices that do not have computers, or their computers are not friendly, the soft-cover texts, A KICK IN THE SEAT OF THE PANTS, or A WHACK ON THE SIDE OF THE HEAD, by Roger von Oech ($10.95 and $12.95 respectively, ISBN 0-06-09024-8 and 0-446-39158-1), provide exercises, stories, tips, and techniques to help you strengthen each of your own creative skills. The books are sold separately, but sometimes you can find them together with a deck of innovation cards, and the set is called a "WHACK PACK." These aids can be used to awaken these skills in your staff, since they are the best problem solvers we have. Then all you have to do is capture the great ideas from the flow of innovation. For those who have an ability to use a computer, friendly or otherwise, some of the more helpful software programs include: * IdeaFisher (approximately $495) contains two parts, the Idea-Bank which cross-references 60,000 words in 700,000 ways, and the Q-Bank which has 3,000 very specific questions designed to help you solve common business problems involving product lines. Available in IBM PC and Macintosh versions from Fisher Ideas Systems, 714/474-8111. * Namer (approximately $195) can help name products or services; it encompasses all kinds of product categories, but it is really best for naming health care products and high-tech services. It will combine root words related to those fields and come up with 200-300 possible names. Available in IBM DOS from Salinon Corp., 214/692-9091. * Idea Generator (approximately $195) combines seven brainstorming techniques to take your answers and reintroduce them as questions that force you to view a problem at a greater depth. Available in IBM DOS from Experience in Software, 415/644-0694. * Mindlink (approximately $499) uses a "mental gym" to warm up your mind with creative exercises, then the program runs you through a disciplined, step-by-step problem-solving activity. It forces you to remove yourself totally from the problem. Available in Macintosh from Synectics, 802/457-2025. * Inside Information (approximately $119) is a very new desktop accessory that contains 65,000 key words and their definitions and related concepts. Available in Macintosh and IBM DOS from Microlytics, 716/248-9150. New software to enhance creativity and innovation comes out every week. There are many other products coming available to help problem solving, innovation, and creative thinking for the average computer user. It is a smart idea to stop at the local software store and discuss your needs with a hacker on the staff. Do not buy the software product until you have booted it up yourself, fed in a current problem or idea, and see what the program can do for you. Not all programmers have the same logic tree as you, and very few understand health care delivery, much less veterinary medicine. These programs are just a logic tree that can be used by most decision makers who want assistance in innovative and creative thinking.
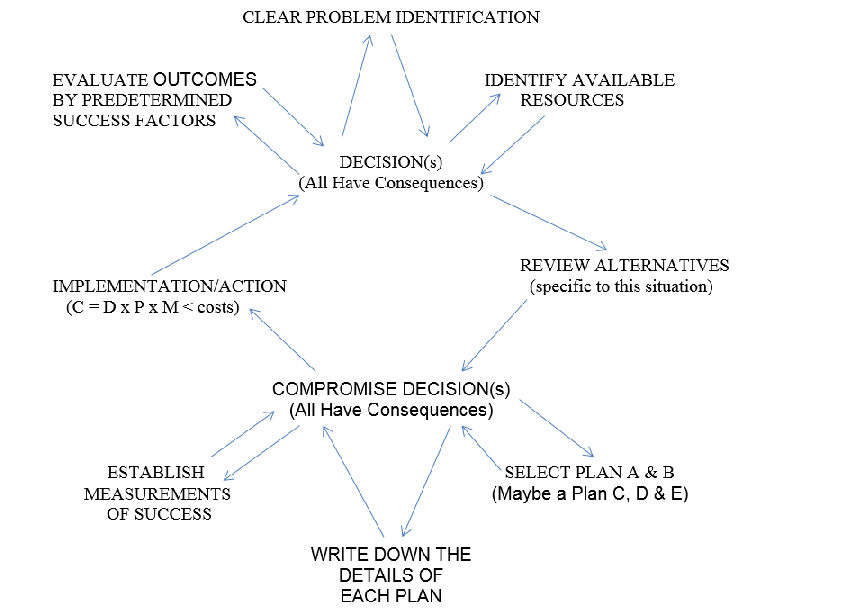
Problem Solving Process - VCI Veterinary Leadership Pocket Guide
DOING GETS IT DONE
When a project stalls, making a new beginning can provide the spark that lets a project catch fire. Inactivity leads to inertia, then the consultant must be called in to break the paradigms which formed the inertia. Picture your practice as a giant boulder resting on level playing field. Time has caused it to settle into a depression. With all the strength available, the boulder may only be moved an inch or two. If something isn't immediately added to the depression, the boulder will return to where it was. On the other hand, if something (e.g., an idea rock) was added to the void created by moving the boulder, it will not be able to return to the "old position" and just sit there. Each movement of the boulder allows another idea rock to be added to the temporary void. In time, the depression will be filled with new ideas and the boulder will be moved on the level playing field in whatever direction is needed, and with a lot less effort than ever before.
With or without an electronic computer, use your brain's natural logic for a five minute "boulder moving effort" when searching for the breakthrough or follow-through ideas. If you are stuck, agree with yourself that you will start to work on a task at a particular time and will continue for five minutes. At the end of the five minutes, determine if you want to continue another five. Make the same determination again, and so forth. This enables you to take focused action rather than view the project as behemoth and helps to build immediate response rewards. If all else fails, stop, relax, and remember the words of Isaac Newton:
"If I have ever made any valuable discoveries, it has been owing more to patient attention than to any other talent."
July 2014 VETERINARY PRACTICE IMAGES Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com
"He who knows much about others may be learned, but he who knows himself is more intelligent. He who controls others may be more powerful, but he who has mastered himself is mightier still." Lao Tsu
In a brainstorming session with other consultants, we looked at the average veterinary practice client cycle and counted the moments of truth that any practice could possibly influence. While all the ideas listed here will not fit every practice, the majority should. The challenge is to get the staff members to accept the responsibility to improve the image in each area they touch. They need to have pride in what they do, moment by moment, to affect these moments of truth. To establish that pride in performance is the challenge of leadership, but that is a different article! Most of the concepts discussed below are expanded in the new Blackwell/Wiley & Sons Press three volume text series, Building The Successful Veterinary Practice, and the sequel, Veterinary Healthcare Services: Options in Delivery. Look at these opportunities, and discuss them with your team:
Finding the Practice (you need to ask this question of ALL new clients to compile these answers) Social Media Yellow page ad Referral by friend/client Newspaper ad Community literature source Referral by out-of-state veterinarian Outdoor signage Ancillary pet supply referral Staff community service Community activities/Rotary/Scouting/women's clubs/government
The Initial Contact Phone for a price quote Phone for a service quote Phone for an appointment New Client Newsletter (mailed post-phone contact) Directions to the practice Stopping in for a tour Meeting a staff member out in the community Meeting the veterinarian at a community function Actual appointment hours offered
Arriving With the Pet Practice identification Direction signage for parking and entrance Parking lot appearance/tidiness/potholes/debris/droppings Access to the front door Entry ease and protection of pet from other patients Fear Factor enhancements Lighting/security Initial waiting room impression (smell, sight, sound) Access to the front desk Staff appearance Decor/odor/noise/cleanliness
Client Relations Specialist (Reception) Staff Courtesy/attentiveness Friendly/smiles Responsiveness/caring Pace/professional approach Phone techniques Gossip level Talk about pets/clients by name rather than condition Bond-centered Practice Approach Waiting time (a maximum of seven minutes) Amenities available Other clients entering and exiting (satisfaction)
Initial Client/Patient Movement Methods Appearance/uniforms/shoes/personal composure Personal hygiene/makeup/hair/breath/face hair Escort to consultation (examination) room Initial interview techniques Hands on pet within 30 seconds Fear Free aspects Nurse (Technician) appearance Body language/voice tone Staff competency Paraprofessional rapport Bond-centered Practice Approach Wellness examination Diplomas on wall (staff and doctors) Odor/cleanliness/noise
Veterinarian Initial Impact Appearance/personal composure Treatment of staff Respect for Outpatient Nurse comments Self-introduction Touching the animal Listening technique Body language/voice tone/rate of speech Terminology Explanation of consultation/examination/findings Patient advocacy/speaks of pet's needs/ensures client decides Bond-centered Practice Approach Empathy/concern for client's position (feelings and fiscal)
Consultation (Examination) Room Exit Summary of findings Staff Training to administer treatments Bond-centered Practice Approach Explanation of charges Prequalify each departure with the three Rs (recheck, recall, reminders) Escort to discharge Protection of animal during transit through hall/reception area
Discharge Actions Attentiveness at discharge/waiting time Discharge desk clutter/appearance Cleanliness/odor/noise Presentation of invoice/bill (consistency with estimate) Collection of fees (some practices have the nurse do this in consultation room) Dispensing medication Concern for client understanding Plan for next contact Bond-centered Practice Approach Establishing the three Rs compliance expectations (recall, recheck, remind) Privacy/courtesy/caring Literature offered to ensure family understanding
Post-discharge Follow-up telephone call by nursing staff Quarterly Informational Newsletters Sympathy cards/memorials for deceased pets Thank you correspondence Health Alerts (Volume 3, Building The Successful Veterinary Practice) Satisfaction surveys Reminders Recurring social media
Over one hundred moments of truth were listed above and the ability of the veterinarian to directly alter them accounted for only about ten percent of the total. The balance are done by staff, and the effectiveness is directly proportional to their level of training competence. Many practices have not yet discovered the value of team-based training, facilitated by veterinary-specific team-based trainers (e.g., see www.drtomcat.com). The amount of concern (training and rehearsal) exhibited by most veterinary practices does not equal the importance of these client impression opportunities.
Consider the moments of truth from the client's perspective. How many times can your staff, facility or practice methods offend their impressions of your practice before they are no longer a client? Conversely, when staff members feel proud of the practice and the healthcare delivery philosophy, every moment of truth is an opportunity to cement the doctor-client-patient bond.
In fact, as proven in most every service industry, how the operational managers and supervisors treat the staff will determine how the staff members treat the clients. When Carlzon asked the SAS headquarters staff what their "mission" was, it took three weeks for the team to decide it was "the movement of people." They closed the headquarters for about six months and took the client-centered service to the field and impressed every one of the 40,000 employees with their importance in the moments of truth. In two years, SAS went from a failing airline to one of the top three income producers in Europe; five years later it was failing again because the leadership appeared over-impressed with their initial effort and did not continue the client-centered emphasis on all programs. They forgot to look into the future and make the SAS employees responsible for changes in the future (there was NO continuous quality improvement). SAS lost money.
American examples do exist, like Marriott, Nordstrom, Worthington Steel, Federal Express, and American Airlines, but they are the exception rather than the rule. In industry and corporate America it has been called Total Quality Management (TQM). Authors like Juran, Deming, and Crosby have made their consulting fame by basing their approaches on reintroducing employee-based quality and pride factors to American corporations. They believe that when the employee puts pride into their daily effort, when they are empowered to make changes for the betterment of the team without first climbing the supervisory ladder for permission, the output will be perceived as quality. The successful veterinary practice empowers its staff to react and change to meet the client's needs. The staff member needs to have the freedom to commit resources without additional line item permission and to make the client perceive a caring staff and a quality healthcare facility. In human healthcare this concept is called Continuous Quality Improvement (CQI).
Assigning accountability to an employee (empowerment) must be accompanied by the needed authority, and these must be supported by job/task ownership. The staff member must think of the practice as "our practice/our hospital" at every decision point in the process. In the consulting business, we find that practice "luck" is usually directly related to the preparation of the staff to grab opportunity as it comes knocking. Where does your practice approach sit in the scheme of things when it comes to preparing your staff to grab the moment of truth and turn it to the practice's advantage?
During the 1970s and 1980s, the veterinary client-centered trend in the United States inched away from client service in the quest for high-tech and personal specialization. However, the 1990s rediscovered the importance of service to the client, and client-centered service was rediscovered (and the AVMA even published an outstanding series of workbooks to help their members relearn this critical business facet, but very few used the AVMA texts as team-based training workbooks to establish an enhanced practice culture or solidify the practice philosophy). The new millennium and the GFC has demanded this facet for success be tailored to multi-generational expectations, including high tech savvy and proactive social media outreach!
The practice that best controls its respective moments of truth will become different from other practices in the mind of their community. These astute veterinary practices will succeed where others have floundered because practice quality and client impressions are communicated during the moments of truth and have very little bearing on the professional facts. They will become the leaders in the veterinary marketplace as we emerge from the GFC, using new millennium techniques.
June 2014 LEADING A MULTIGENERATIONAL PRACTICE TEAM Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com
You have to get different generations communicating so they can appreciate what each seeks and why, as well as identifying what they hold in common. Only through facilitated dialogue, where individuals feel listened to, can different generations within the practice team discover common ground. Tom Catanzaro, DVM, MHA, LHACHE
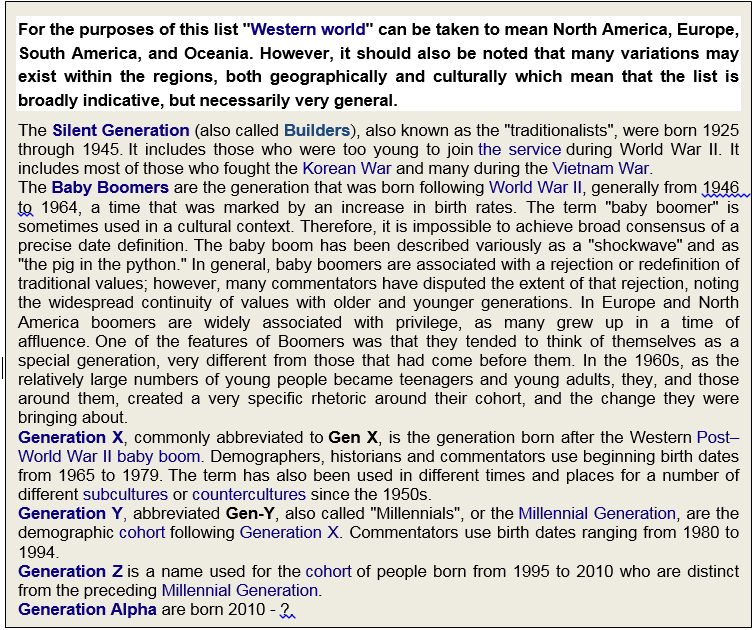
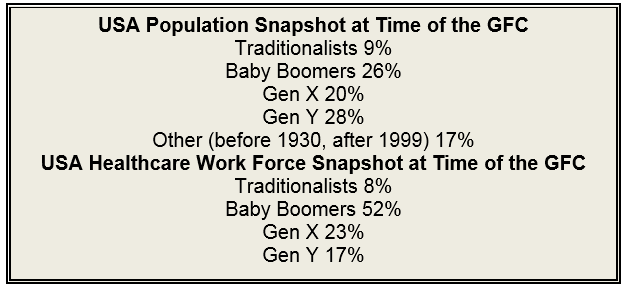
In very leadership course I have ever staffed, or developed, communication is defined as the "getting and giving of information." In most veterinary practice settings, the doctor has learned to talk "at" the staff members (that is how they were taught in school) rather than with them, and the ownership ensures the manager delegates processes rather than outcome tasks. This is now compounded by the generational differences seen within veterinary practice teams, which gives the organizational behavior and practice culture more stumbling blocks than answers. Currently, most multi-doctor veterinary practices have a staff comprised of four generations: traditionalists, baby boomers, Gen-X and Gen-Y. The difference in attitude and in value hierarchy among veterinary practice providers of different generations is so great that practice owners and younger staff often fail to even hear what the other is really saying. The older embers members of the staff believe the younger members have no work ethic, while the younger members of the practice team suggest the old timers should "get a life." But these obstacles can often be removed through facilitated dialogue that builds trust and enhances mutual understanding.
Traditionalist practice owners and Medical Directors were born at the end of World War II, and for them, veterinary medicine was a vocational calling. Their profession and self-identity are one in the same, and in their eyes are analogous to James Herriott, a priest, a rabbi, or other minister of the flock. Traditionalists respect hierarchy; join civic, fraternal, and professional organizations; are seldom computer literate, and would never imagine requesting reimbursement for being on call.
Baby boomer veterinarians learned from the traditionalists, so on the surface, they appear a lot like the guys who taught them their craft, often in ambulatory medicine settings. However, they work with a different set of motivation factors: the acquisition of material wealth is core to their practice approach. That attitude is particularly evident in the latter half of the baby boomer generation. Younger boomers are sometimes labeled the "Jones generation", as in "keeping up with the Jones." For the boomer veterinarian, failing to work generates feelings of guilt. The younger Baby Boomer veterinarians are loyal, do not fear taking on debt, do not tend to accept statements of authority, are not joiners, and are not likely to sacrifice personal pleasures for the good of the group.
Generation X are significantly different from traditionalists and baby boomers. For Generation X, managing time and balancing life are primary values; being part of a veterinary team is only a small part of the existence and self-identity. They are equally vested in life or lives outside the practice, and for that reason, prefer known shifts. Gen Xers are transactional and seek immediate stability, looking for what they can get for working the prescribed shift(s). They do not tolerate governance well, have a lack of trust in managers, supervisors/or even practice leadership; they are loyal to principles, not organizations.
THE NEW MILLENNIUM
A unique phenomenon occurred in the American workplace, especially in healthcares settings, as we entered the new millennium. before the new millennium, most leaders and employees shared a common generational attitude - they were most all part of the baby boomer generation. This congruence of generational attitudes clearly led to a more positive work environment and a more aligned and engaged work force, yet as we entered the new millennium, it all started to unravel.
Although Baby Boomers will continue being the primary practice owners and Gen Y associates, colleagues, and staff coming into their sphere of influence. The trend slowed when the GFC struck, and baby boomer retirements were postponed, but the economic restraints are changing again, in time, the generational shift will occur to Gen-X and Gen-Y values.
When Baby Boomers entered the veterinary workplace, the leadership was dominated by traditionalists who saw duty, loyalty, and sacrifice for the good of the practice as part of the definition of their practice existence. baby boomers saw working hard as a means to personal growth, career development, and an extension of their ambition. As Baby boomers began to dominate the workplace, it led to tensions, and even the split in expectations of "early baby boomers" from "late baby boomers" . . . the disengagement from the practice workforce was perceived by many traditionalists as disloyalty, and major discord followed. Generational differences impact communication styles, technology needs professional development processes, workplace expectations, compensation & benefit needs, desired leadership styles, and the effectiveness of reward and recognition systems. Generations tend to agree on achievement and a desire for credible, trustworthy leadership.
Practice leaders who understood that their management styles needed to change thrived in the new multi-generational environment, while those who continued using approaches and techniques from their own past found their ability to lead and motivate greatly diminished; in fact, many of the older styles have been reclassified as "Bullying", and legal workplace actions are being taken at an ever increasing rate.
Today, progressive practice leadership needs to take specific steps to stop the perception of Bullying and prepare for the changing dynamics of the modern veterinary healthcare team.
STEP ONE - Acknowledge the Need for Personal and Organizational Change. When managed and led appropriately, a multigenerational practice team can be the springboard for greater collaboration, unique exchange of ideas, and a more productive practice. While I outlined the generations earlier, the Gen Z is not yet in the veterinary workforce, except for maybe a work-study student, yet they will cause another shift in leadership and organizational behavior change needs.
Just as the days of one-doctor veterinary practices are coming to a close, so is the traditional doctor-centered healthcare delivery systems. Veterinary extenders are needed in today's competitive professional marketplace, which requires different training system than the traditional "see one, do one, teach one" attitude of the baby Boomers and Traditionalists. Training to level of trust is a slow and often computer based staff development program, requiring practice duty time be adjusted since Gen X and Gen Y seldom take work home. Assigning small but meaningful application projects to newly trained staff requires time and resources be allocated, as well as the "question being the best answer" in many cases; these efforts require special public recognition, for the effort, the milestones reached, and the success measures met in the process. The next step is program accountability, aligned with the interest area(s) of the developing staff member ; again, time, and resources will be required, as well as mentor support (never bullying).
No single style or approach exists for successfully leading the multigenerational practice team. The leadership must adapt to meet the individual needs of all generations. Leading while preventing intergenerational conflict requires encouraging self-identification within the practice team, and subsequent training opportunities. Acknowledging generational differences enables a greater appreciation for values, characteristics, and experiences that help shape the work ethic, motivation, and ideology of the practice team members. Developing innovative solutions to address the value-based needs of each group makes it possible for practice leaders to improve the organizational practice culture, staff motivation, and personal engagement.
STEP TWO - Develop Specific Strategic Assessments and Responses To optimize human capital, today's veterinary practice leadership must understand what attracts, engages, and retains distinct generations that comprise the modern practice healthcare delivery team. Key human capital components that will drive the engagement and motivational culture of the practice team include:
STEP THREE - Time Implementation Right! In life, as in making leadership decisions, timing is everything! Strategic assessment leads to strategic response, which comes from analyzing and reporting on catchment area demographics and trends. New metrics are needed for measuring progress and achievement of new programs; old metrics give rise to regression and frustration.
Most successful practices survey their staff on a regular basis to determine organizational climate, as well as assess the intergenerational issues and healthcare delivery program effectiveness. These surveys should be designed to take advantage of knowledge, strategies, and tactics related generational differences and SOC compliance perceptions in the practice's team-based healthcare delivery programs, for instance (but not inclusive):
By recognizing the need to change, by developing plans now that may require months to train staff and implement effectively, and by engaging each person in a distinct generational modality, "where they live", practice leaders can best meet their responsibility to their associates and team members - creating the right environment, enhanced organizational climate, and individual opportunities for self-esteem while delivering high levels of client-centered patient advocacy for clinical, operational, and financial excellence.
May 2014 LEADERSHIP FOCUS INSIGHTS My first text was BUILDING THE SUCCESSFUL VETERINARY PRACTICE: LEADERSHIP TOOLS (Volume 1), my thesis for my masters at Baylor University was based on tracking leadership evolution in the past 100 years, and I have staffed over 19 weeklong leadership courses (only 1 in veterinary medicine), so it is safe to say I have been a student of leadership for over a quarter century. I cringe at many seminar speakers who seem to promote themselves as experts, with no credentials except the PR to get podium time. At a recent conference, I was recently asked what I saw as major focus areas for leaders. There are many things a leader needs to balance, and besides for the Balckwell/Wiley text, I have three monographs on the subject in the VIN bookstore, but here are a few key things I believe that they should always keep front of mind. Create Focus: A leader should strive to paint an inspiring vision. Most people don't want to run from something, but rather they seek to run to something. As individuals, we want to be a part of something greater than ourselves. A leader should paint this inspiring vision, and then articulate the priorities to help people know how to make progress against that vision. Fall in Love with the Problem, Not the Solution: It’s human nature to love our own ideas. In our associations, it is usually the STRATEGIC PLAN, most often written for 5 years and forgotten/outdated within one year. That means that we hang on to those ideas for too long. I promote Strategic Assessment and Strategic Response for practices at the community level (yes, there is a monograph on that subject in the VIN bookstore). Along the leadership or innovation journey, you must ask: Are we making sufficient progress to believe that our original hypothesis is correct, or do we need to make a change? If you never lose sight of the problem, how you attack the solution can remain more flexible, iterative and ultimately, be more likely to succeed. Lead With Questions Not Answers: The best leaders don’t need to have all of the answers. They surround themselves with great people, and ask the right questions. When doing a practice consult, I get many of the best "turnaround" ideas from the staff members; I use my 2000+ practice experiences to translate that into proactive programs. It’s not what you know. It’s the questions you ask that help you become a more effective and inspiring leader. Build Capability Through Principles & Frameworks: Leaders must unpack “WHY” a decision has been made, and not just the “WHAT” the ultimate decision is. The next step is to ask the staff teams within their own zones to develop the WHO and HOW. This practice makes explicit the principles or criteria that you applied to reaching a conclusion. At this point, the WHEN becomes a joint decision, and includes milestones and success measures (which do not change during the implementation process). These principles can then provide teams with a compass to navigate uncertainty and make their own decisions when you are not available or able to assist, moving beyond your individual ability, and building organizational capability. Cast a Tall Shadow, Not a Dark Shadow: All leaders cast a shadow. The question is whether yours is blocking the sun, or inspiring others with its silhouette to strive for more. As a leader, we must all walk the talk. Leaders need to role model the behavior they want their organizations to emulate. The two greatest indicators of what we view as important are (1) how we spend our time and (2) the questions we ask. Organizations watch these cues to determine what leaders “really view as important”. So be clear on your say/do ratio, and ensure the shadow you are creating is the one you aspire to project. All that said, if I had all the answers, there would not be 989 leadership and management texts on the bookstore shelves - they would only stock mine. Not hardly folks. Situational leadership and situational management are both an art and science. To adapt a consulting program to any practice requires flexibility and depth of knowledge most neophyte consultants have not yet attained, but they will under-bid my rates for two main reasons: 1) they want the practice booking, 2) they don't value their own knowledge. Organizational Behavior (a recent VIN Bookstore monograph) lies under most practice programs, and forms the practice culture. This cannot be changed by a consultant, only by the practice owner. My job is to mentor the practice owners, and in turn, the practice staff, to move the practice to the next level. In all honesty, about once every two years I have had to disengage from a consult because the owner believed in disposable staff or otherwise was a control-oriented boss who was not willing to change one iota. In those cases, when I am on-site and discovered these type situation(s), I disengage and only charge direct expenses and NO TIME FEE. I do have available flexible time for consulting in the next couple months . . . but then I start to travel - in July I head to Japan for a HAB speaking engagement, in August I am on VCI Seminars at Sea (Alaska) with 7 other consultants as faculty (new faculty details and revised seminar agenda is at /site/view/214832_.pml if you would like to participate in this "mountain top" adventure CE experience), then in September I am speaking at he Kentucky VMA Annual meeting, and follow that in October, with speaking at the Wild West Veterinary Conference in Reno, Nevada. I hope to be booked for some consults in coordination with the last two engagements, if we can coordinate the desired dates. Also please note, a new post-GFC economical consulting program has been added to the web site this month. The attached article is actually the proceedings from a conference I did in Australia a couple months ago. People who have come to my seminars over the years know my proceedings are "additional information" and NOT an outline to follow as I speak - they are designed to stand alone and help the reader gain insights to the topic at hand. I believe the attached article expands well on the Leadership Focus Insights offered above. Hope to see you on a consult (including the new economical regional program just added to my website) or at VCI Seminars at Sea (Alaska in August), but regardless, sure hope the attached article helps you see some alternatives for possible use in your practice. Tom Cat >*-*< May 2014 Attachment PRACTICE TIPS & TRUISMS Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com If you want to go fast, you go alone. If you want to go far, you go together. For the record book, ideas I am about to share will be contrary to some of your opinions of what a veterinarian-centered practice should be doing. Some of the ideas will be contrary to your levels of trust. Some will walk away saying it can never happen on their watch. In short, many veterinarians CRINGE at the thought of sharing these ideas; that is called ‘university training’ and has proven to be short sighted in most other healthcare professions. Think of a “high powered” dental practice, where you are booked to see a dental hygienist every six months. Next time you do, ask them to let you look at the appointment log. The dentist may have 3 to 5 chairs scheduled for his restoration work, and depending in the practice, there may be 6 to 12 hygienist chairs, which also now do whitening. That makes 9 to 17 appointment columns per dentist. Sure, the hygienist columns only reflect about $180 per hour production potential, while the restoration chairs are producing $300 to $600 per hour for the dentist. In these ‘high powered’ dental offices, you will notice an administrator coordinating all the business activities. You should also note the extenders working the restoration chairs with the dentist, skilled at getting X-rays as well as molds of the teeth and arcades. Now think of your practice with one column per provider and ask yourself why have you been limited by the expensive “practice management business software”, which by the way, cannot even do the basic business formula of ‘Income minus Expense equals Profit”. And you pay how much for that set of limitations? So today is may be the time many of you get to move the next level . . . Take M-2-D Next Level The ideas may make some of you cringe – you will cross your arms, lean back in your chair, and say “no way!” That is YOUR CHOICE. I have been in 2000+ practices, and will be sharing concepts that have worked in Australia, New Zealand, Japan, Canada, USA, UK, and Northern Europe. The CHOICE of which ideas will be yours and yours alone . . . but a word of caution: Never try to implement more than 3 new ideas at a time (within 1 month), and for best results, restrict them to one per practice zone at a time. TEN TIPS & TRUISMS #1. Share the Accountabilities. In any veterinary practice, there are more requirements than most people realize. I have watched veterinarians change their own light bulbs, open their own mail, snake their own toilets, and otherwise do jobs that reduce their income production potentials. Attached is a list of accountabilities, and while you may not be excited about sharing some of these requirements, the simple fact is if you do not, they will all take you off line, and you lose $200-$400 an hour from outpatient and $300 to $700 an hour from inpatient production, if you let yourself get distracted with these accountabilities. You were trained to do them by the school of hard knocks (they were not academic subjects, nor are they journal worthy articles in most cases), so it is self-evident that you can train others to be proficient in any of them! #2. Develop Program Managers. In my world, coordinators are the link pin in zone operations, the ‘coordinate the people’ in a practice zone (client relations, outpatient, inpatient, animal caretakers, etc.). Program managers are the ones that ‘coordinate things’ like inventory, dental care, behavior, immunizations, nutritional advisor, etc. Attached is a functional staff volunteer list, with built-in resources, to start the Program Manager programs when you get back to your practice. #3 – Written Standards of Care (SOC). Whenever a practice extends beyond one vet, a written standards of care is needed, this includes when a practice starts to empower their staff members to represent the practice’s core values, mission focus, and standards of patient care to clients. The AAHA Compliance Study showed that most practices were losing about $630,000 per vet per year by not being consistent in well care and preventive care practices. By writing the practice’s commitment to well care and preventive care in a single, easy to read document, everyone will become aware of the commitment required. The SOC should be the WHAT statements, not protocols and not lengthy WHY explanations – that is for staff meetings when programs are being introduced. Medical record reviews can then be conducted weekly to ensure compliance by each provider to the SOC elements. Every SOC NEED (never use the word ‘recommendation’) is followed by a X-A-D-W; X = do it; A = appoint it; D = defer it (needs until when date); or W = waiver, never mention it again. When doing the quarterly budget review, failure to reach target goals are assessed by individual program and individual provider commitment/compliance to expected SOCs (patient needs) and related booking rates for specific programs. And by the way, with a written SOC document, even the savvy owner should stop making exceptions for his old mates! #4. Share thank you notes. When I was in practice, I had a box of thank you cards, blank inside, with practice specific covers, and scanned the local newspapers for reasons to send a hand-written personal thank you note to someone, whether they were a client or not; any community contribution was enough to get a thank you note! Many people will tell you they have every thank you note they’ve ever received during their professional career. Many practice post their thank you notes on a bulletin board or in a scrap book, but inversely, send out very few . . . that is a very interesting dual standard in my mind. If you ever have mailed a thank you note to a staff member at their home, with a real stamp and hand written envelop, for something they have done for the practice, the team, or yourself, you know the gratitude response first hand; the sad thing is many managers have never seen this gratitude because they have not reached out to say ‘Thank You’ in an unusual but memorable way. Thank you notes put a tangible and meaningful token of gratitude right in the hands of those who need it the most. Is there a staff member in your practice who makes a difference and for whom you are grateful? If so, take a few minutes to write him/her a thank you note, and BE SPECIFIC on the behavior you are accolading. #5 – 2xFL – think two visits a year for life. Most every client knows that one dog year is 5 to 7 people years! Yes, we all realize that it is not that easy, but who cares when the client believes that simple ratio. Most practices have a predominant female client base, up to 70%, who already know they need to see their OB/GYN every two years at least, and their dental hygienist every 6 months. What would be the response if they told their OB/GYN, “See you in seven years doc!” . . . answer, NOT HARDLY LADY! In most all surveys, clients say they don’t come back because no one made it important enough for them to revisit. It did not help that we taught clients to come only for vaccines, and charged prices so high that the wallet exsanguinations stopped vacations, movies, and even happy meals for the kids. Start planning the next visit, even if it is with a veterinary extender who is well versed in well care and FEAR FREE PHILOSOPY of practice. #6 – Use the 4 Rs on every patient every time. The dentist schedules the next visit (6 months or sooner) before your leave the clinic. The pediatrician hands the young mom a handful of lab forms and schedules the next baby visit before the discharge is completed. Your physician should be setting up surveillance visits for your blood chemistries. Your car mechanic puts a tag on your windshield when to come back. The wife’s hair dresser schedules the next visit before she leaves the salon. Heck, even the dog groomer schedules the next visit as a matter of discharge planning. So why do vets NOT practice a similar planning technique? Answer, we were raised by wolves! Actually, we were raised by ambulatory veterinarians who had to deal with producers who put the pencil to the economics of every vet service, so they used the word recommend, and came only when called . . . until the days of herd health and recurring equine dental floats. Companion animal and equine clinicians need to ensure every patient is at least 2 of the 4 Rs as part of every discharge action: Revisit (make the appointment), Recall (expected telephone contact time), Remind (e-mail, SMS or snail mail promise), and Resolved (medical record entry on successful close out of cases). #7. Hire for Attitude. This is NOT the seventh thing you need to do, it is the first thing to do when building an improved practice team. Resumes have become a creative writing art form, they cannot be trusted any more (HINT: always call every reference). In the text, Building The Successful Veterinary Practice: Innovation & Creativity (Volume 3), Blackwell/Wiley & Sons Publisher, there are interview check lists for most positions, with hints on what key words to listen for when assessing attitudes. In training, we talk about KSA-A: Knowledge, Skills, Attitude and Aptitude. Given a candidate with the right attitude, training the skills and knowledge becomes easier. When they seem to come with skills and/or knowledge, but do not have the aptitude or attitude, training is very difficult if not impossible. For every person departing the practice team, it is an opportunity to seek someone with the attitude and aptitude to fill a void or shortfall on the team – do not look for clones! In fact, in the VCI Signature Series monograph, Staff Orientation & Training (from the VIN bookstore, www.vin.com), there are self-directed training programs for empowering the staff members who have the right attitude and aptitude. #8. Train to Trust. There is no “average” in healthcare skills or knowledge, no adequate, nothing that is the ‘fair’ or ‘good’ category of assessment. Competency is Excellence, there is no other grading system. Think of placing an I.V. – what is a “C” average, maybe going through both sides of the vein? Think of a femoral bleeder, spurting a one meter arc – what is a “C” average for stopping the bleeding, maybe a 10 cm arc (this still leads to a body bag)? Think of placing an anesthetic misadventure (what surgeons call an animal that stopped breathing while on the table) – what is a “C” average, maybe inflating the apical lobes only (this still leads to a body bag)? Think about “partial pregnancy” – there is no mid-ground, it is ALL or NOTHING in every case. In recurring performance evaluation assessments, why “grade” past performance instead of planning for the next 90 days? “Remember what you did last month – well don’t do that again!” does not build a proactive relationship, as opposed to, “What do you want to change, or learn, in the next 90 days?” The latter allows you to be a mentor, and share accolades while in route to the next level of exceptional performance. In fact, studies have shown annual reviews are worthless, and prospective quarterly performance planning is what works with the current generation of healthcare workers. In fact, in the VCI Signature Series monograph, Staff Performance Appraisals and Planning (from the VIN bookstore, www.vin.com), provides individual forms for each zone in the practice, as well as manager and veterinarian forms and formats, for self-assessment and goal setting for the next 90-days. #9. Understand the Power of the Human-Animal Bond (HAB). Interestingly, the ‘Human-Animal Bond’ terminology came into vogue with the Delta Society and Dr. Leo Bustad, back in the early 1980s. Then by 1990, the American Association of Human-Animal Bond Veterinarians (www.aahabv.org) was formed (only a $35 membership fee). I am a Charter member of both, as well as a past Board member of VetOne, a veterinarian-industry cooperative of the late 1990s. HAB spawned the bond-centered practice, which then became the client-centered practice, and is now the Pet-centered FEAR FREE practice. My most current FEAR FREE contribution is the VCI Signature Series monograph, Building the Bond-Centered Practice (from the VIN bookstore, www.vin.com), updated in 2013. Concurrently, my text, Promoting the Human-Animal Bond in Veterinary Practice is now in the Second Edition (circa 2009), with all 26 appendices (mostly staff plug-n-play type ideas) with the new well care chapter (250 pages); the good news is that it can be obtained for FREE – and you should be able to afford FREE. The book is posted in the VIN Library (www.vin.com) for FREE DOWNLOAD – it only takes a half ream of A4 paper. #10. Become a Student of Leadership. I advocate being a continual student of leadership . . . a good leader must be able to manage, but a good manager may not have the slightest idea about leadership. I once had a CFO approach me and wanted to blame another Director for an operational shortfall, yet I would not participate in the “blame game”. She returned the next day as offered to take 20% of the blame, if I would support her effort in passing 80% of the blame to another Director, again I asked about ‘future think’ and would not play the “blame game”. On the third day, the CFO offered to take 60% of the blame if we could shift 40% to another Director; I again told her that if she wanted to work on future prevention, alternative solutions, or even reorganizations, I would participate, but I would not enter into the “blame game”. She never understood; she was “bean counter” to her core! In the 2000+ practices I have visited, I have learned something beneficial in every one, usually from a staff member. My first text was, Building The Successful Veterinary Practice: Leadership Tools (Volume 1), three of my Signature Series monographs specifically address various leadership aspects within a veterinary practice, I have written three separate leadership courses in three different countries, and in the 19 weeklong leadership courses that I have staffed or led, I have learned something about the inter-relationships of the leadership skills, and the inherent understanding of participants about the human nature leadership. In my text, The Practice Success Prescription: Team-based Veterinary Healthcare Delivery, available for FREE download from the VIN Library (www.vin.com), it comes together as an essential element for a cohesive veterinary practice development plan. In simplest terms, the WHAT and WHY must be shared by the leader as a new concept is shared and before a program can be moved forward. The WHO and HOW must come from the appropriate staff members working in the zones to be impacted. The last step before any implementation is determining the WHEN, a joint agreed upon set of milestones and success measurements. A good leader does not unilaterally change the target in the middle of an implantation effort. A manager will often take credit and give blame, but a true leader will take the blame and give credit to others. You can manage programs, yet you must lead people. Listing ten tips and truisms may sound presumptuous, yet that is the topic the AVBA assigned me. My preference is to enter into the practice fray and assist a practice team and its leadership to assess the organizational behavior, work through the issues at hand, and move the practice to the next level – this is what tailored consulting is all about! It is not an overnight fix, nor can it be done by adding some gimmicks; most of us have tried that and found the choices wanting, and the apparent solutions unlasting. Any of the above tips should be tailored into your own practice philosophy, core values, and mission focus; they must become part of the ordinary and not be seen as passing “tests”. Speaking of "tests", I have included a self-assessment for PROFESSIONALISM as a leader in your workplace at the end of this article. Have fun!
VETERINARY LEADER PROFESSIONALISM SELF ASSESSMENT The following characteristics relate to professionalism in the veterinary workplace. Answer these questions to see if you exhibit a high degree of veterinary professionalism. Answer yes if you demonstrate these characteristics or behaviors at least 90% of the time. 1. Do you have all the skills required to be successful as a practice leader? If not, are you in the process of learning them? 2. Do you communicate (verbally, visually, and in writing) well with others? 3. Do your managers deem your behavior to be professional? Does your manager and zone coordinators approve of your attire, the hours you keep, the way you conduct yourself in general? Does he or she seem comfortable coming to you with special projects or to discuss problems or ideas? 4. Do you have a high level of integrity? Do you tell the truth at work? Are all clients treated (and charged) the same. Do you see personal tasks through to completion and avoid cutting corners? 5. Do you practice the Golden Rule? A true professional treats others with respect and expects the same from them. Do you return borrowed items right away and in good order when you’re done using them? 6. Do you live up to your commitments? In any leadership role, you agree to do certain tasks and assist/mentor others. Some tasks you must do routinely, without asking others to take on your responsibilities; others you delegate the outcome accountability and become a mentor (e.g., not taking them back). A real test of your professionalism comes in your ability to meet all these commitments while upholding the standards of quality and timeliness set for your practice team. Individuals with a high degree of professionalism make promises to themselves and to others about what they will and won’t do. They keep those promises. 7. Do you report to work at the agreed-upon time (or early), ready to work, and with a cooperative and positive attitude? Do you willingly pitch in during times of staffing or other crises? Do you keep the team informed when you will not be available, and return on time ready to work? 8. Do you avoid conducting personal business while at work? 9. Do you take full responsibility for the results of your efforts and actions? 10. Do you have a quarterly performance planning process in place in your practice, and ensure it operates effectively by monitoring target action progress? 11. Do you have a your own quarterly performance plan and continually seek self-improvement and self-awareness by looking for opportunities to enhance your professional growth? 12. Do you take pride and satisfaction in the work you do, both clinically and operationally? 13. Do you actively participate in one or more professional organizations? 14. Do you keep confidential and staff assessment information confidential? 15. Do you avoid "telling" and "berating" of staff (e.g., the bullying method you saw as a student at veterinary school clinical rounds)? Are new programs 16. Is your practice the employment of choice for veterinary staff in the community?
Mid-month April 2014 I am here in Australia and Easter is coming - big weekend here - so everyone asks "What are you doing for Easter?" Funny thing - no kids so no eggs to be hid. No family, so no trips to be made. I am at the age of reminiscing, and my mind goes back to Montana in the 60s, where Easter was spring skiing - shorts and a sleeveless sweat shirt on the sunny slopes of Bridger Bowl. I had Head 210 GS skis for the snow in the bowls, and 3' shorties for the groomed slopes. It was an interesting time, since a Canadian fraternity brother from Banff (Calgary) taught me to ski early on, and I was instructing the beginners at Bridger Bowl (the Bridgers are a unique east-west stretch of Rocky mountains, so there was north facing slopes - meaning GREAT POWDER). So why do I regress here? When teaching skiing, you have to get people to lean forward (which when rushing down a mountain side, seems crazy). The exception is when skiing deep powder and you have to float your tips, hence my Head 210 GS skis. But I regress on my regression. Most beginners just will NOT lean forward, it feels awkward and scary. I have watched even intermediate skiers on the intermediate slopes going downhill without leaning forward - they think they know better than the experts. When you lean forward, you are committing to the slope, and instead of coasting, you are carving your turns on the mountain. The stakes are higher - the decisions you make each second are crucial . . . you are fully engaged with the sport, the each at mountain, and with yourself. Unfortunately, many skiers never learn to lean forward. Leaning back is easier, simpler, and feels safer. It feels more natural (especially if your are a Queensland water skier). Yet, this resistance to leaning forward leads to mediocre skiing. I wrote the text, The Practice Success Prescription: Team-based Veterinary Healthcare Delivery, VIN Press, circa 2009, and it is in the VIN Library for free download. Yet it requires the practice leader to "lean forward" as they change their practice culture, and most do not. They download the book and try to 'cherry pick' ideas, rather than committing to the adventure by leaning forward and craving their course into that mountain. The last two Fortnightly Newsnotes included articles on interpersonal skills, mentoring and bullying, but to embrace those concepts, practice leadership to commit to changing the practice culture and organizational behavior paradigms (a new Monograph in the VIN Bookstore). That is not unlike leaning forward when skiing, and in most Baby Boomer led practices, the leadership is NOT leaning forward and NOT committing to carving a new course down the mountain. The reasons are many, but it often comes down to the mentor selected for the practice leadership and practice culture redesign - most Baby Boomer led practices do NOT invest in a qualified veterinary savvy consultant, and if they do, many still revert, even after seeing their staff get excited and fired-up with the new accountabilities of team-based veterinary healthcare delivery. Leaning forward is scary! Change is scary! Altering the interpersonal skills, mentoring and organizational behavior paradigms is NOT easy if you have never done it before. I am always amazed at the veterinary leaders who use bullying styles instead building better relationships (e.g., Crucial Conversations and Crucial Confrontations, by Patterson, et.al.). The authors of Crucial Conversations didn’t set out to write a book on communication; rather, they began by researching the behaviors of top performers. They found that most of the time, top influencers were indistinguishable from their peers. But as soon as the stakes grew high, emotions ran strong, and opinions differed, top performers were significantly more effective. What the authors observed during this study and captured in this runaway bestseller is a distinct and learnable set of skills that produce immediate results. The attached article take sit up a notch. Centers of Excellence is a foray into larger general companion practices (multi-doctor) as well as emergency and specialty practices, and discusses how to work and play well with others. Sure sounds like "leaning forward" as you start carving a course down that mountain; and I am available for helping the transition occur in your practice. Please note - I have added a new, economical, regional practice assistance program to my Australian consulting options, which could be exported with some coordination, titled: TIME TO SMILE AGAIN (/vci-programs.pml) Have a Happy Easter, and please remember, rabbits are NOT allowed in Queensland - signs are posted at the NSW border for rabbits that can read. But there is a QLD movement to recruit Bilbies (rabbit bandicoot). :>) Tom Cat >*-*< Thomas E. Catanzaro, DVM, MHA, LFACHE P.S. VCI Seminars at Sea (Alaska cruise in August, with a faculty of 8 Internationally-savvy speakers) would be a great opportunity to start that "lean forward" transition for yourself. Details are posted at /site/view/214832_.pml. As an alert, the following was just sent by our cruise coordinator, Randy Norris, to a recent inquiry (randy.norris@frosch.com): We have limited availability on the cruise, but I do have a few balcony staterooms available. Total cost per person, including all port charges, government taxes, transfers to/from the ship and gratuities…$2,223.53. This quote does not include airfare. We also are offering an optional pre-cruise tour of Denali and a post-cruise tour of the Canadian Rockies. If you are considering something else, please let me know. PLEASE - Book now and avoid being squeezed out of this great CE adventure! Mid-month April Attachment: CENTERS OF EXCELLENCE People are like stained glass windows; they sparkle and shine when the sun is out, but when darkness sets in, their true beauty is revealed only if there is light within. Elizabeth Kubler-Ross Why in the world would a consultant who wants to talk about “centers of excellence” start with a quote from the leading author in Death, Dying and Grief? The answer is basically an observation of what has been happening to our profession. The Veterinary Teaching Hospitals (VTH) used to be our “centers of excellence,” yet all the recent studies show new graduates are not prepared for the real world of practice. They have amassed a significant debt, and have not learned to influence decisions by clients for the welfare of the pet. Most all of the new graduates, interns and residents seem to understand the esoteric logic of academia, but have not learned how to work and play well with others; most would have a hard time getting a “D” in sandbox play. This is also seen in many of the specialists leaving academia, since they were the “trainers” of the interns, residents, and new graduates. THE TRUTH OF THE DEMOGRAPHICS A true center of excellence is more than large facilities, good doctors, and expensive equipment. We cannot expect people raised in academia to understand the business and client relations required in private practice. Just about four decades ago, before the expansion of the clinical-based board specializations, many land grant, college-based Veterinary Teaching Hospital (VTH) professors had come out of private practice and into the teaching hospitals; now they go from graduation, to internship, to residency, to academic appointment, to tenured professor, so personal clinical productivity is no longer an expectation. Concurrently, while the Veterinary Teaching Hospitals have become centers of excellence for tertiary care, some of the privately-owned specialty practices are becoming the centers of excellence for profitable veterinary business models. A true center of excellence requires the presence of an integrated program of delivering quality health care, including the ability and commitment to measure quality of care on a continual basis and compare it with an external benchmark; high levels of client satisfaction due to better continuity of care; availability of a more comprehensive array of services; ability to handle the full range of complications; and lower cost based on improved efficiency and productivity through the implementation of standards and staff-based facility operations.
THE BOARD’S ROLE Leadership and performance assessments have become established business tools, but are still rare occurrences in healthcare, veterinary or human! Many veterinarians avoid feedback on performance, or go through such assessments without a clear idea of the process and how to maximize the feedback they receive. Many times this has been caused by the sender, who is going through a process they have read about without really understanding the core elements of the philosophy. For ANY assessment to be successful, it is important to define expectations up front, take an active role in the nurturing and developmental process, and then to build on strengths as the assessment process is shared.
The current management guru thinking is that the most comprehensive assessments give you feedback from different types of people - including your direct team, your peers, lateral service specialists, and the administrative supervisor(s). Sad to report, for Gen-Y staff, it is often from their peer group from social media, totally uninformed individuals supporting the Gen-Y staff member's perceptions of "fair". The real assessment should have a broad enough base to allow open feedback, such as - career development, intellectual abilities, management style, team skill development, interpersonal communication styles, emotional profile, and personality/behavior make-up and traits. In the normal world, this is called “open feedback,” in management it is often called “360 degree assessment,” and in the practice, it is usually called “a pain.” Regardless of what you call it, after it has been done, you should be able to: ? Select the right organization for the feedback. It is important to select the facilitator and individual(s) who will conduct the feedback exercise. This is not a project for the “do it yourself” practice manager. The organization should have a history of facilitating the feedback process in veterinary medical situations, they need to respect the social contract associated with healthcare delivery, and they must appreciate the “calling” which most veterinary professionals and paraprofessionals carry with them into this career. Most important, the facilitator should have a personal style with which the Board is comfortable. One emergency practice we deal with has caused the referring practices in the community to increase the use of TKO fluids (to keep open), just because they send virtually every animal back to the referring practice in the morning with I.V. systems flowing. These emerging progressive and patient-centered type practices, which do not mediate the standards of care based on outdated paradigms, become a benchmark for the professional community as well as client community. The staff gains pride in the continuity and standards of care, and clients perceive that pride as quality; most clients will pay for quality as a value, since it provides a peace of mind towards the animal they steward. Peace of mind, that is all that we "sell" at a center of excellence; all else the client is allowed to buy for their surrogate family member. End of March 2014 In the last Fortnightly Newsnotes (Ides of March), I attached an article about I.Q. vs E.I. - and that got me thinking, which is usually dangerous for someone. While most vets have a high I.Q., or at least a very high academic history, E.I. is NOT a given. When I was doing a seminar for the CSU Veterinary School students, one approached be after the seminar and said, "By what you said, we have to deal with people as veterinarians, I may be in the wrong profession, I am in veterinary medicine so I only have to deal with animals!" I nodded and said she was correct, and no animals carry wallets or credit cards, so she had to deal with people if she went into practice. Her follow-up was equally interesting, "So, it looks like I have to go into research." I explained to her about boards, supervisors, and even in academia, colleagues. Her response was as expected, "So what am I supposed to do? I have spent 7 years of University pursuing veterinary medicine and I am about to graduate in a year, and I do not want to deal with people!" My answer was simple, I told her to join Toastmasters, or take a Dale Carnegie course, or maybe get some personal counseling, since people will always be in her future once she leaves the hallowed halls of academia. That got me an unexpected response, "Oh, that's right, I could get an internship and residency and stay within academia!" My response was, "Students are people!" and she responded,"But no one cares if a professor does not relate well with students, and the reciprocal is true, no one cares if students cannot relate well to to the world." On the 2000+ veterinary practices I have visited, as well as the 19+ week-long leadership courses I have staffed, the major variable is E.I. (Emotional Intelligence). In fact, in most cases, the core issues lie with the practice owner, Medical Director (often the same person), or practice manager (who has usually been trained by the practice owner, who has not had management or leadership development experiences except at the school of hard knocks). Practices have the staff members they deserve (they have been hired, trained, and retained) and the clients they deserve (they have been courted, oriented, and retained). Then they invite me in and want me to change everything they have built, without changing themselves. My consulting engagement letter now says, "If you do not plan to change, do not invite me into your practice." When we build a veterinary healthcare delivery team (the 500 page book is in the VIN Library for FREE download, www.vin.com), we first train the staff to a level of being trusted, then build a mutual respect by using small 'outcome oriented' tasking, with accolades by the practice leadership for the journey as well as achieving the milestones and approximating the expected success measures. After that, we empower the staff member(s) to develop a program within their interest area, and give them the resources (time, money, Internet sources, etc.) to develop and implement a client-centered, patient advocacy, program plan. Again, we do this with accolades by the practice leadership for the journey as well as achieving the milestones and approximating the expected success measures. It is only after these sequential steps that true team harmony starts to surface, and that then lends itself to inter-team synergy and an enhanced practice culture, which lends itself to the improvements in productivity and performance. What do we usually see when a practice is embarking on this journey without a mentor? 1) Practice owners cherry picking the 500-page reference, and skipping steps, and then wondering why no one is moving forward as desired. 2) Medical Directors or managers tasking process, rather than outcomes, and then wondering why there is no initiative for continuous quality improvement (CQI). 3) Staff members who have been "burnt" before, so they lay back and internally think, "And this too shall pass." With tenured staff, this is often the discussion outside the practice setting. So the attached article is about mentoring; the good, the bad, and the ugly. And yes, I am available to sign-on as a practice mentor (consultant, see my web site, shown below, for the current time-based fee details), so the journey does not have to be an exercise of frustration. If you have never been there, and have never developed a true team-based veterinary healthcare delivery team system, step-by-baby-step, please do not embark on the journey in the dark. Please, get help (the VCI Seminars at Sea 2014 would be a great synergy time, information below). I am available on both sides of the Pacific pond. :>) Tom Cat >*-*< Thomas E. Catanzaro, DVM, MHA, LFACHE ALASKA - Adventure CE - AUGUST 2014THE BEST FAMILY & TEAM REWARD TRIP EVER!
End of March Attachment: Mentoring Mania MENTORING MANIA Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com “The mediocre mentor tells. The good mentor explains. The superior mentor demonstrates. The great mentor inspires.” Dr. Tom Cat Students graduate from veterinary school and are told to find a good mentor for their first job. The academics don't tell them, and the students fail to realize, mentoring is NOT core subject in veterinary school, nor are there progressive continuing education courses specializing in making doctor-centered veterinarians acutely aware of what mentoring is all about in today's professional arena, nor are there course that teach the skills and attitude needed to be a great professional mentor. THE TWO-WAY STREET Mentoring is a two-way connection based on trust, honesty, and competencies. Agreed upon expectations and boundaries help manage the balance in the mentor-mentee relationship. My own understanding and experience for mentoring relationships started at the Academy of Health Sciences, in a one-month, full time, faculty development program, and has been honed over many leadership courses, as attendee, faculty, and course director; I have never been involved in a course or consult where I have not learned something new about mentoring and leadership. In short, mentoring relationships ensures that both parties are accountable, responsible, and engaged, and have a few basic "rules" for the process: 1. Only mentor people who take the commitment seriously and are action oriented. 2. Teach mentees how to think, not what to think. 3. Ask a lot of questions. 4. Listen carefully. 5. Keep advice simple. 6. Build on strengths to counter weaknesses. 7. Hold people accountable, e.g., "When will you . . . ?" 8. Set expectations, "What will success look like?" "What happens when you succeed?" "What does failure look like?" 9. Stay involved. respect appointments to meet, overlying schedules, and engage in Q&A, listening! Don't just commit the time - commit the energy! 10. Consider the whole person, including home life, hobbies, and outside interests. Are any affecting performance or concentration? 11. Hear their caring intentions, don't make them wrong when an idea is shared. My favorite tool in mentoring is to use literature, and teach mentees how to research, challenge, and think for themselves. When assigning a project, refer to a history, or biography, and prepare yourself for some interesting revelations. Ideally, a mentor should always work on becoming a better mentee, and a mentee should work on becoming a great mentor. Different mentors, however, have different attributes - no one has all the answers. It is possible that you may be unable to provide the right guidance for any number of reasons. Look into yourself and acknowledge, if that is the case, that the maximum benefit is not there for the mentee. Give him/her permission and time to seek another relationship that may be of assistance. Sometimes, having two mentors simultaneously can be of benefit to the mentee. One from inside the practice, and one from outside the practice (maybe from Rotary or elsewhere in the community). First and foremost, the mentee must be comfortable and relaxed with the in-practice mentor; the outside mentor may make the mentee uncomfortable, since they may not respect the paradigms and excuses found inside the practice. The tension in this arrangement keeps the mentee on their toes and makes them high conscious of personal behaviors, as well as highly focused on the discussion at hand. It will take an extra effort to address the assignment(s) and ensure the quality of the finished project or final discussion summary. TELL-TALE SIGNS THAT INDICATE YOU ARE NOT A GOOD MENTOR When he came out of surgery, no one was standing around; in fact, the entire staff had all disappeared. I was consulting in a two partner practice in Texas, and noticed that a busy inpatient team vanished when one partner was about to emerge from surgery. I finally found the staff gathered around a picnic table on the back of the property, and asked them about the exodus. They were honest, That partner would come out of surgery and reroute/retask everyone without even asking what they were doing. It made for a very fractured work day, not to mention a very poor practice culture. The other partner, who was a great outpatient clinician, when confronted with this syndrome, tried to make excuses, but when I would not accept the excuses, decided they needed to have a crucial confrontation (Patterson's second book after Crucial Conversations); I provided him the text. Are you a mentor that loves to tell stories about your own successful cases, or maybe your hobby, or even your pets? Do your team members make lame excuses to avoid you? Have you tried empowering your trained and trusted people, just to revert and take back all decision making, returning to the traditional control-freak mode of a doctor-centered practice? Chances are, if these things are happening, you are the problem, not the solution. Here are a dozen various tell-tale signs (they all do not have to occur within your style for mentorship to be negated): People's eyes glaze over, they do not make eye contact, and some even yawn when you are pontificating. You notice that no one asks questions to clarify what you mean about any item or project. Colleagues invite others into the conversation with you, then soon disappear. You talk incessantly about your subject of choice, never asking of an opinion or input. You spend too much time in communal areas, like hanging out in the break area or around the front desk Staff members find a reason to leave when you enter the break area. You have a list of petty complaints about the practice operations, and never hesitate to air them publically. When not in surgery, you spend your day looking for ways to make your days more interesting. As a manager, you seem to delight in listening to practice gossip. You know very little about the staff members, but they know a lot about you! Staff members in the break area put on their ear-buds as soon as you enter the area, or pretend to be talking/texting on their phone. Staff brainstorming energy reverts to safe program tweaks, and the staff starts to wait for the new ideas to be issued by the owner again. FEEDBACK LOOPS When I ask any mentees what matters most when leading a project team, I often hear about connections between people, not the crunching of numbers. Successful leaders excel in empowering others to assume management/project leadership by asking, "What do you think needs to be done?", not "What do you want to do?" This type question sets the stage for mentee to prioritize milestones and success measures, not his/her own engagement. Effective mentoring improves productivity; it strengths skills be reinforcing lessons already learned. It helps others recognize their own special gifts and potentials; it builds confidence, and more often than not, it teaches both mentor and mentee new things about organizational behavior (see Signature Series monograph of that title in then VIN Bookstore, www.vin.com). If your mentoring efforts are done with an honest commitment to others (sometimes called "servant leadership", a term coined by Bob Greenleaf in 1970, made popular by Blanchard & Hodges in 2003, and expanded by Sipe and Frick with the "7 Pillars" in 2009), you will find mentoring brings personal enrichment, revitalizes your day, and provides an enduring sense of accomplishment as you follow the personal growth of mentees and the practice team. Ides of March The Ides of March (the "middle of March") is the 15th day of the Roman month of Martius and is most closely associated with Julius Caesar - it was not a good day for Julius - he got stabbed 23 times by his "trusted" friends on this day in 44 B.C. - most of us know how that feels. I was just asked this past week to submit an article to a national magazine on comparing practices. At best, comparisons are odious. How would you compare an apple to a watermelon, since they are both red? How would you compare a sea slug to a Great White Shark, since they are both live under the surface of salt water? How would you compare one-doctor veterinary practice, in a one exam room leasehold facility, with two part-time staff, in a depressed catchment area (family income 30% below major community average), with most clients having less than a high school education, to a progressive, six consult room, free standing, three doctor practice in an upscale community with an average "college degree" client base? The article for this Fortnightly is discussing Emotional Intelligence (EI) instead of IQ, since the depressed community EI may in fact be higher than that of the upscale community . . . and the practice that underestimates the HAB and EI of their clients will likely plateau and wither away. I have seen it happen, and in one case, the consulting client forbid me to discuss programs when trying to rally support from her tenured staff. Three months later she came back and asked "Which Programs should we start with to get buy-in". The challenge was deeper than that - she had hired technicians who were all breeders, so they naturally answered all questions on the phone and kept clients from coming into the practice. We had to find programs for each staff member that would require them to bring clients into the practice. In another recent practice consult, we were converting from a spay-neuter practice to full service, but referral of well-care issues to staff was not occurring. We first issued pocket notebooks to each staff member, with programs across one margin and provider vets along the other, and each week, notebook pages were provided the manager to count the in-house referrals, and veterinarians who had swore to the SOC well-care compliance issues yet had no referrals to staff had the opportunity to meet one-on-one with the medical director/practice owner, to discuss their SOC compliance rates and well-care commitments. This required a confrontation, which most veterinarians try to avoid, so I had the leaders read Crucial Conversation by Patterson, et. al., and made them address the practice health vs "nice guy" paradigms. When the smoke cleared, it was all EI factors! Hope you enjoy this edition, and please think about the Alaskan Seminars at Sea 2014 in August, (/site/view/214832_.pml), since these type issues can become your tailored open one-on-one discussion time to help YOUR practice. The optional pre-cruise rail trip to Denali and the optional post-cruise trip to the Canadian Rockies are added benefits for making this a family outing to remember . . . adventures like this make continuing education a memorable time.
Ides of March attachment: Interpersonal Skills IMPORTANCE OF INTERPERSONAL SKILLS Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com For most people, Emotional Intelligence (EI) is more important than one's learned intelligence (IQ) in attaining success in their lives and careers. EI is the ability to monitor one's own and others' feelings and emotions, to discriminate among them, with an ability to read signals from other people, and use this information to guide one's interpersonal relationships, actions and thinking in an appropriate manner. Steve Bressert & Kendra Cherry We have heard it before, but it bears repeating: Studies show at 90 percent of veterinary practice leadership failures are attributable to shortfalls in interpersonal competencies - factors such as leading team-based healthcare programs, developing a positive work environment centered on clear Standards of Care, retaining inspired staff, developing respect and trust, and coping with change. The message is clear - if you are going to excel as a leader in a multi-doctor, team- based, veterinary healthcare delivery system, you must master the "soft skills" of caring leadership. In veterinary healthcare management, where the basic unit of business is the person (stressed client or caring staff member), these skills are even more important, it is a shame that it was not in the basic curriculum of veterinary school. If the veterinary healthcare providers on your practice staff are spending time replaying a conflict in their minds, their energy is directed away from patient care and client-centered service. If you lack the "soft" interpersonal skills to motivate your frontline healthcare delivery staff members, including fully accepting the written well-care Standards of Care (SOC), as well as the optimally using the new information technologies, your practice could be missing revenue opportunities and/or negatively affecting patient outcomes and client perceptions. CLIENT PERCEPTIONS Research shows that an unhappy client will tell about 13 others, each of which will tell 5 more (that is a 60+ potential client negative impact), while a satisfied client will convey their pleasure to only about 6 others. The traditional internal practice justification "they do not understand" does NOTHING to change the practice's downward spiral reputation in the community (primary catchment area). While in most communities we expect about 30 new clients per month per FTE veterinarian, and we measure "word of mouth referrals" from satisfied clients to ensure we are getting over 50% of new clients from satisfied client referrals, this yardstick is seldom used as a gauge of "soft skill" effectiveness. Emotional intelligence - however "soft" it may seem - has a direct effect on aspects of the practice as concrete as patient safety, client perceptions of clinical outcomes, staff pride (which client's perceive as quality) and profitability. The following is a closer look at the FIVE CRITICAL interpersonal competencies. KNOWING YOURSELF It sounds easy, but in fact, self-knowledge is challenging for most veterinarians; we were all raised in a "no error" academic culture, so blaming and rationalization seem to reign supreme. To truly know ourselves, we must become aware of our blind spots, those situations we don't handle as well as we should for optimal business performance. For some practice owners, this involves failure to listen to the viewpoints of others, for some it involves making tough decisions with appropriate urgency, for others it concerns difficulty motivating their own staff. One tendency I am seeing more often is the GEN-Y leader sharing her thoughts out loud (as if they were on Facebook or a smartphone network with peers), which staff members perceive as a plan in the making, and when the thought/dream disappears, the staff become disillusioned; false starts actually cause reserved acceptance of all new initiatives by staff members. Most veterinarians, especially in Australia, have a tendency to sweep shortcoming, as well as personal weaknesses, under the rug rather than cause a confrontation. Yet inevitably this backfires, the rug gets too lumpy and people start to trip over the accumulated shortfalls being ignored. When weaknesses are ignored, we are also ignoring how they affect others, whether we are overtly aware of the challenges or not. Self-knowledge enables you to recognize your weaker areas and take corrective action. MAINTAINING CONTROL Most veterinarians believe that they maintain control; they were trained in case management where all control must lie with the attending provider. Yet challenge is that the staff members may not agree with the practice owner's self-definition. The key here is to be aware of when you are losing control. Do you pause and reflect when you are entering that territory that is difficult, or does your voice get louder and your understanding of others diminishes? Is your tendency to overreact or under-react? In a large facility I had developed, we also did the community animal impoundment (and adoption), and one of my credo positions was NEVER will I see inhumanity in my practice culture. We had a new kennel staff member decide it was easier to power wash the run with the animal still in it rather than change the animal to another run when cleaning (per protocol); when I caught this individual power spraying a run with a dog still in it, I shut the system down and physically escorted him through the clinic and out the front door. The word went out - do NOT ever be inhumane to an animal in this practice! While the occasional outburst can be attributed to being human, if your personal pattern is seen as more extreme - if you are perceived as becoming overly upset or shutting down - you are undermining your own effectiveness. MAINTAINING MOTIVATION Motivation is a combination of optimism and perseverance from inside an individual; again, our professional education has usually based on a "bell-curve" academic logic and fear of failure. Studies have shown that most people have a biologically based "set point" for optimism; when selected to veterinary school, that optimism is very high, and during the professional years, fear increases by an average of 25%. Some people look at a glass as half full, others think it is half empty; very few accept that the glass is full, and only the ratio of the contents may vary. Reality encompasses all three perspectives, yet the more positive the assessment, the better leverage the leader has. Optimism cascades own to those you are leading, enabling them to stay motivated and positive; the more positive a team member is, the more motivated and tenacious they will be in reaching for enhanced outcomes. When managers are habitually pessimistic and primarily critical, the followers become less innovative and more risk-adverse. Perseverance is the second part of the motivation equation. A leader must demonstrate the ability to stay on course through thick and thin, setting a clear vision of where the practice is headed in the long run. RECOGNIZING OTHERS' INTERESTS Good leaders have the ability to take a win-lose situation and craft at best a win-win solution, or at the very least, a tolerable outcome perception for all involved. When seeking a transactional attorney for my consulting team, it was almost impossible to find an attorney who understood WIN-WIN - attorneys are raised in a WIN-LOSE culture - but for partnerships, I needed a win-win mind set on our transactional attorney; I eventually found one and we developed him in veterinary medicine, where he has been recognized a yardstick of excellence, and was eventually elected to the Presidency of the USA Consulting Association, Veterinary Partners. To recognize the interests of others, you must know the needs and perspectives of all the parties involved (perceptions play a large part in the formation of perspectives). Only with this level of insight can a leader create buy-in and get the team members behind the practice agenda. Rather than attempting to control the process every way, which only alienates the followers, a savvy leader defines the WHAT with clarity and provides the WHY in a logical client-centered patient advocacy manner. The great leader then gives the team members ample time to develop the WHO and HOW, as it pertains to their practice zone(s) and their perceptions of client-centered patient advocacy. Then the legendary practice culture allows ample time for leaders and followers to come back together, set the WHEN, including training time, starting point, realistic milestones, and measurements of success. Remember the famous adage, "I must know where my people are going so I can run ahead and lead them to a successful completion." COMMUNICATING FLEXIBILITY Flexible communications is the hallmark of great leaders. When developing the Leadership Training Course for Belize, we introduced the concept of "ARF" in the interpersonal relations leadership skill, and participants really grasped the concept. You could hear "ARF" coming from campsites throughout the jungle; "ARF" stood for Absolute Rigid Flexibility. Leaders must be able to adjust their communication style according to the needs of the situation. This involves being aware of the effects of your words, as well as the tone of your voice, on each specific audience you encounter. For example, managers often misjudge the powerful impact of their words and emotions on their team members, communicating with them in the same way they would with a well informed peer. But new and unsure staff members are less likely to push back, challenge, or even seek clarification from their leaders, which all too often leads to miscommunication and feelings of alienation. This one-way "communication attempt" is not true communication; communication is the getting and giving of useful information. Talking "at" someone inevitably increases the relational "static" and slows practice progress, often derailing effective outcome results and smashing any feelings of personal pride. BUILDING INTERPERSONAL SKILL SETS Good interpersonal skill sets are built over a lifetime, but there are several steps you can take to start building these skills faster and more effectively: TALK WITH YOUR TEAM Teach those around you to give you open, honest feedback about your leadership style. That means NOT disagreeing with their assessment, but rather, saying thank you in a caring manner. Tell them what areas you are working on and enlist their help. You might not always get the whole truth, but just demonstrating that you are trying to improve your emotional intelligence skill set can help your team improve their performance as well. READ I like to start practices with Bracey's book on Managing from the Heart, Paterson's text on Crucial Conversations, and a few of my Signature Series monographs from the VIN Bookstore (www.vin.com), but there are a myriad of articles and books on communication skills and emotional intelligence. Many of these references provide strategies for real world situations such as resolving conflict or motivation of the team. The simple act of reading about emotional competencies will increase your awareness of behavioral expectations for becoming a "best practice". DEVELOP MIND MAP BRAINSTORMING METHODS Tony Buzon has the easiest texts to understand mind mapping, and my text, Building The Successful Veterinary Practice: Innovation & Creativity (Volume 3), Blackwell/Wiley & Sons Publishing, not only describes the process for veterinary practices, but also ends each chapter with a mind map for the reader's completion. Remember, when brainstorming, there is NEVER an assessment in an idea or input item, and if it sounds "off the wall", it goes into the parking lot in the corner of the mind map so it can be recalled for later(even if it is home phone call to "bring home the milk"). Mind maps are built and expanded upon by the group, and then people get to sleep on the ideas, and readdress the mind map on the following day. Eventually, the mind ma is transferred to a project sheet (format is provided in the Leadership Action Planner monograph, VIN Bookstore). COMPLETE FEEDBACK EVALUTATIONS The concept of the 360-dgree feedback has often gone astray since they migrated from positive to negative feedback items. If you desire a 360-degree feedback system, keep it sweet, short, and to the point, addressing the positive attributes of the individual an what could be improved with expansion. There are many on-line sources, but as a caution, do NOT use a negative feedback format; this is the time the primary stakeholders get to build on what is good about someone. Other type assessments include personality and behavior self-surveys; behavior can be a term of employment and effected by the practice culture, but personality cannot be changed from the outside. Self-assessment surveys can often help alert the caring user to blind spots and opportunities for development. WORK WITH A SAVVY VETERINARY CONSULTANT/LIFE COACH External feedback can help you develop perspectives that you might not have addressed previously, and if it is a savvy veterinary consultant, add some team-based training awareness to enhance productivity within the practice operations. A life coach is usually not veterinary savvy, but they are insightful in helping you identify areas where your emotional intelligence skills can have the greatest impact on those around you. While the life coach will help you identify strategies for self-improvement, a veterinary savvy consultant can tailor programs to enhance team strategies to enhance communications and awareness for improved client-centered patient advocacy programs. Whether you have a life coach or a savvy practice consultant, or both, there needs to be follow-up for plan implementation as well as evaluation of progress. Ultimately, your success in interpersonal competencies is determined by the experience of your stakeholders, whether than be stressed clients, concerned staff, or caring family members. No matter how effective a communicator you believe yourself to be, if your front line providers, your management team, and as applicable, your board, do not feel the same, you are NOT maximizing your leadership potential.
End of January/ Beginning of February 2014 Sorry about being a bit early with this edition - my relocation next week has Stop Telstra Internet and a Start Telstra Internet with a Telstra service delay expected - I requested services be transferred from my current location to the new location - not a big deal in the USA, but in Australia - different story! So I requested the STOP to be 31 Jan and the Start to be 28 Jan - but Telstra has not standardized their systems, so the two houses are on different equipment - even handled through different service branches within Telstra - Australians are saying, "yes, so what did you expect?" and Americans are asking why do we tolerate this problem - 8 hours on the phone to get a START without a guaranteed 'no penalty' STOP. Everything is scripted in Telstra, so no one has to be accountable for the answers - not unlike most software service points. I have discussed the Tall Poppy Syndrome (TPS) of Australia and New Zealand before, and now, some psychologists are stepping in to define why people are underachievers, or at least, why they do not want to be "stars" in their chosen fields - don't you love it when psychologists try to explain the TPS without stating the obvious. Unconscious Forbiddance vs Peter Principle - tale of two cultures Unconscious Allegiance or Loyalty Suppose a very gifted and intelligent individual grew up in a family, a religion, a culture (e.g., Australia) that preached "modesty," "humility," and danger in standing out (e.g., Aussie TPS). In the young person’s mind, especially before the age of seven when the brain can finally begin to make personal evaluations, these messages are received and stored in the unconscious mind as "The Truth." But what happens when their manager or boss sees their greater potential and promotes them to a quite visible position where "modesty," "humility," and "not standing out" are impossible? It may look like the "maximum incompetence" version of "The Peter Principle" as that individual starts to decline in professional execution, strategic thinking, timely planning, you name it. But they will not be exhibiting incompetence, rather they will be attempting to get the job done within the bounds of their unconscious allegiance or loyalty to what they learned way early on about the rules of good and expected behavior that are now long standing residents of their unconscious. Judith Sherven, PhD and her husband Jim Sniechowski, PhD http://JudithandJim.com have developed a penetrating perspective on people’s resistance to success, which they call The Fear of Being Fabulous. http://OvercomingtheFearofBeingFabulous.com OVERVIEW ARTICLE So I thought the article I would attach to this Fortnightly Newsnotes would center around Emotional Intelligence (EI), as opposed to IQ (all vets have a respectful IQ, that is why they got accepted to veterinary school); TPS is more of an EI factor. The article is a bit longer than usual due to the combined concept targets, so please bear with me. I also centered many of the examples on multi-vet, emergency, or specialty practices, so I do not directly attack the general practitioner . . . but the principles are the SAME and the learning points are almost identical . . . it is just the multi-vet, emergency, or specialty practices, MUST have effective governance (Boards), and thus are great examples for EI awareness, while single veterinarian practices - a dying breed - do not need it immediately (they just talk to the mirror). This is one area where a savvy veterinary consultant is almost an necessity - and I hope you will see why as you read the attached article. I am moving houses this week, from a high set with no A/C to a low set with 4 A/C units - I cannot beat the Brisbane humidity, so I must find an alternative, but the move will be finished before February, so make me a consulting offer (general scope of my consulting time-cost details can be found at www.drtomcat.com) with a couple weeks lead time, more if you are second or third in the queue . . . I have two potential consults in Sydney/NSW area, one for 3-days on-site and another for a year-long (4 days on-site, then 2-days on site a quarter later, and then 2 more days in about 90 days when the self-directed training has been about completed), but without any retainers, they have no guaranteed sequence in my consult commitment planning. I hope this article helps awaken a few leadership stirrings in your operational practice direction(s), and hopefully, allow you to self-assess the EI of your daily personal interactions/relationships. Tom Cat >*-*< Thomas E. Catanzaro, DVM, MHA, LFACHE P.S. VCI Seminars at Sea 2014 - AUGUST 2014 Agenda, itinerary, and very special faculty bios at (/site/view/214832_.pml) Attachment (Jan/Feb 2014): EQ Evolution EVOLUTION OR REVOLUTION vs. WORKING DIFFERENTLY Thomas E. Catanzaro, DVM, MHA, LFACHE Dipomate, American College of Healthcare Executives CEO, Veterinary Consulting International DrTomCat@aol.com; www.drtomcat.com The future belongs to those who see possibilities before they become obvious. John Sculley, CEO, Apple Computer The days of experience are being replaced by the days of new challenges. The skills and habits of yesterday cannot answer all the needs of tomorrow. Emergency practice went from the “fire engine” production practice, to a “rotary” shared by multiple practitioners, so some could sleep a few nights a week. Then companion animal demands started increasing, and the “rotary” sharing of night call shifted to the smaller critters too. Then some bright young man decided there was demand for an emergency practice, a practice that opened only in the evenings and on weekends, and the general practice doctors happily referred those night calls to the young man who filled a niche market. Then came the specialty practitioner, who could not find a home in academia, and was looking for somewhere to practice his/her trade of highly specialized veterinary healthcare delivery . . . and somehow noticed the emergency practice was not being used during the weekdays. A symbiotic relationship started to form between specialty practices and emergency practices, so facility and equipment overhead could be minimized, as well as 24-hour care becoming available for the specialist’s patients. Ever wonder why some of the most brilliant and ambitious leaders derail their careers, while those with less obvious "I.Q." skills climb the leadership ladder? Since 1987, I have been visiting practices and coaching veterinary healthcare leaders in the 'real world settings' they have created for themselves and their practices. In the early years, I attributed it to lack of exposure to alternatives, since veterinarians seldom stretch outside their own walls - their "knothole" view of the world was usually VERY restricted! But it was not an I.Q. or experiential factor, it was a shortfall in their innate emotional intelligence (EI). Most veterinarians scored well in high school and university entrance exams (those are I.Q. elements), but with a shortfall in emotional intelligence, they ended up inadvertently harming their careers as a result of unhealthy behaviors and habits. Because good leaders, by definition, achieve organizational goals through others, you'd like to assume veterinary practice owners have superior people skills. However, all too often, this is not the case. FIRST - in veterinary school, they were taught they were accountable, 24/7, 365, and were trained in case management - seldom was the veterinary healthcare team ever mentioned, much less leadership skills (most academics have tenure, not leadership savvy). SECOND - when starting a veterinary practice, there is seldom money for staff, so the veterinarian learns to do it all themselves. As they incrementally add staff members, seldom do they consider upward mobility or expanded capabilities of the new staff member; they just look to reduce their own stress and schedule demands. THIRD - most continuing education venues post-graduation are scientific, with minimal hands-on team-building experiences or interaction exercises, so they do not come away with real experiences reflecting better team development. Let's give you a chance explore this further - read the following scenarios and then ask yourself, , "What emotion(s) do I feel?": You were selected to oversee the implementation of expanded practice hours, possibly 24/7, due to your analytical and execution skills. Your colleagues tell the boss that you spend your time lecturing instead of listening to the team members. You interrupt others and work from your own agenda, often putting down feedback as "that is wrong". You are known as the person who always says 'yes' and takes on extra work or completes the tasks of others. You feel unappreciated and burned out. You wish you could have just one three-day weekend to yourself. You are in a meeting and the practice manager, or a colleague, takes credit for your program's success. This seems to happen often, especially with this person. The medical director is progressive and well meaning, often implementing new programs, but sometimes without adequate training and feedback before implementation. The practice manager downplays the veterinarian's lack of people-skill style to his vet-centered history in the practice. You are now "in the middle" and in a quandary of how to provide feedback. There is NO escaping our emotions! Whether we like what we feel or not, we are emotional creatures, especially in a profession which most of us entered as a "calling" rather than an economic windfall decision. Daniel Goleman, author of "Working with Emotional Intelligence" and "The Brain and Emotional Intelligence: New Insights" is the leading authority on EI. Goleman's premise is that sensitivity to emotional states (one's own and others) and effective relationship skills (EI) are critical competencies in today's healthcare environments. But wanting it does not equate to getting it. The essence of EI is awareness, transparency, and vulnerability. EI is the ability to cope with setbacks, remain optimistic, elicit charisma (positive attraction) and stay purposeful even when things are not going well. EI does not mean that you have to be "soft" or "emotional." EI simply gives you the tools to identify and build on strengths (yours and others), remove barriers, understand limits (yours and others), focus on solutions, and when necessary, call the foul!
FOUR CORE EI SKILLS
ENTER THE EXPANDED-HOURS DRAGON The new era of veterinary specialty has been prompted by organizations such as VECCS, and the “out of hours” emergency practices have been giving way to 24/7 Urgent Care facilities. Sharing facilities format have given way to building mega-facilities to house all the specialists and the Urgent Care services. The only facility problem is that the academic Veterinary Teaching Hospital (VTH) is the wrong model for a private practice, multi-specialty complex. Teaching hospitals need hallways to move large groups of students, and to divide research fiefdoms for tenured professors. At construction costs which often exceed $150 a square foot, hallways and circulation space need to be minimized, receiving and treatment support must be centralized between the occupants, and there needs to be a single Board controlling the policy and precedent of the facility. This has not been taught in our VTH environments. I consulted with a small, one-doctor, leasehold practice, in a depressed community, which had plateaued for 18 months. Since most clients commuted to work via bus or train, weekdays were slow, yet Saturdays were pure chaos. We empowered the team, got them to buy-in to the new vision, and trained them as veterinary extenders with in-house training programs as well as outside wet labs. We then embarked on appropriate pricing dental prophys, DG1+ and DG2+, for the staff to complete while the veterinarian was doing outpatient services and other duties. We built up the liquidity so we could hire a client relations specialist, and then a part-time associate. Once the part-time associate was integrated into the Standards of Care and practice's operational culture, we moved the operational format to include Tuesday and Thursday evening hours (Wednesday was a big community church night and welfare checks came on Thursday). We increased liquidity so the part-time associate could be full time (yes, it was trial and error finding the right person), with each vet working about a 35-hour week. Saturdays were less chaotic, and Tuesday and Thursday nights became busy outpatient times. In one central hospital, when we entered as consultants to do the feasibility assessment, the existing ophthalmologist stated very clearly that he did not need any other member of the complex and would not participate in the rental of the common use or shared use areas. It only took the new board a few months to see the fallacy in that logic; the new replacement ophthalmologist has been cooperating very well ever since. In a multi-practice owned central emergency hospital, surgical space was utilized by the owners of the outlying practices. They were supposed to schedule the surgery space use, but a few always wanted “drop-in” privileges, and came in as “owners” and redirected operations to their own benefit. A few others wanted to handle their own early evening emergencies at their own clinic, and then refer later in the night, yet they wanted a full share payment for emergency use and kept reducing central facility staff so there was more profit. We were called in by the Executive Committee due to the dysfunctional operations. We found that while the lack of core values was the key source of the problem, lack of Executive Committee support for the operating standards was what was draining the staff and the liquidity. The “inmates were ruling the asylum,” and the Executive Committee did not want to address the issues. We developed a Governance Board structure, core values, clear policy and precedence for operational delegation to the hospital administrator, and a routine follow-up system to ensure the new Board kept their word until they learned the new ways were better. In one multi-specialty complex, when we were doing the utilization review for a new facility, the radiologist thought he was the center of the world, just like when he was a tenured professor. He did not understand that radiology was usually a support function for most healthcare delivery in a multi-specialty complex. He even demanded that every X-ray taken be read by him, and he would bill all the specialists for this service . . . we had the board buy all the radiology equipment and then tell the radiologist what the utilization plan was going to be. We were conducting a follow-up consulting program a multi-specialty practice, and Dr. DTC, ACVECC, was brought along to provide some emergency and critical care development in the emergency practice staff of the complex. During the after-hours training, Dr. DTC noted the sound of animals in pain, and offered the surgeon his assistance. The surgeon deferred assistance. A few minutes later, the sounds of pain again penetrated his training mode, and he again offered the surgeon assistance in pain management; the surgeon again declined. This exchange was repeated a few more times, with the same non-responsiveness, and as we departed for the evening, Dr. DTC requested my opinion on how to deal with a specialist who was also the owner, and yet neglected pain management. I suggested a quiet one-on-one the following morning, between the surgeon and Dr. DTC. Long story short, after that meeting, it is one of the quietest specialty practices we consult with, and pain is no longer an acceptable option with any patient. A governance Board system could have addressed this if the standards of care had not been so closely controlled by the owner/surgeon. In one emergency hospital, established in a store front leasehold, an opthomologist wanted to lease the clinical space during the day. The emergency practice was shareholder-owned, and the share holders saw it as a “profitable offer.” It took two years to get the flow established so the specialist was clear from the facility before the emergency team started operations. If there was an informed governance board, these issues would have been established before the first day of occupancy. One well established multi-disciplinary specialty practice contracted with a veterinary architect to design their new building, and by the time the planning smoke cleared, the specialists had added over 20% circulation space so large hallways could divide their areas . . . they needed an experienced consultant to save them that cost, which now, after a couple years of occupancy, they are scratching their heads at the cost of all that wasted space. In an effort to “save time,” the board had made the decision to use the expertise of the architect, who gets paid based on the cost of the facility, not based on the effectiveness of the plan. A second opinion from an established veterinary consultant, with facility management certification (e.g., Board Certification by ACHE), would have saved 20% of the multi-million dollar cost of construction, a great return on investment. These are all issues where a clear and well-developed governance board could have been used to resolve the issues. Most shareholder boards of multi-practice facilities or emergency practices, just want a return on their investment. Some want to milk the cash cow out every month, and there are a few shareholders who want to take hands-full of hamburger out of the cow while it is being milked out by the other share holders. These examples are not usually the people who want to ensure quality healthcare, or even an appropriate practice/facility culture. Board members must leave their own shoes at the door, and assume the role of a practice advocate when they enter the board room; the board ONLY exists between falls of the gavel. SIX TARGETS OF OPPORTUNITY Our veterinary healthcare system is fundamentally flawed in its design. It relies on outmoded methods of work, such as linear scheduling of doctors as if they were still driving utes (pick-up trucks) from farm to farm. The system set up for the staff support has often been a failure, as with doctor-centered practices scheduling based on doctor whims versus facility capabilities and staff becoming veterinary extenders (e.g., seen as ward/service-specific nurses, nurse practitioners or physician assistants in human healthcare). Practices hire people for their strengths, provide inadequate in-service training, pick on their weaknesses, and then blame them for shortfalls; when anyone ”blames,” they abdicate personal accountability for resolution. We have already proven that working harder will not improve quality, while concurrently it has proven that it can disrupt over 50 percent of the families. We can learn to work differently, and it must start by redesigning the systems that we have become so comfortable with over time. To aid in the transformation of the current systems, we have started to publish the VCI Signature Series monographs for the “do it yourself” veterinarians. In the case of governance boards (Leadership Action Planner monograph and Chapter 2, Veterinary Management in Transition: Preparing for the 21st Century, from Iowa State University Press), they must focus and align their environments toward providing healthcare delivery that is: Safe: as Dr. Bill Kay always said to the incoming AMC residents, “First, do no harm” . . . avoid injuries to patients and staff from care and services intended to help them. The practice’s Safety Committee must be empowered to be an active sentinel of dangerous conditions. Effective: providing services based on the best scientific knowledge to all who could benefit, refraining from providing services to those not likely to benefit (avoiding under-use as well as overuse of available equipment). Client-Centered: providing responsive care that is respectful and responsive to the client’s needs and values, while ensuring that patient welfare guide all clinical decisions and care (give two “yes” options - usually time of access choices - record waivers and deferrals). Timely: reducing wait time, implementing nurse-centered triage programs, avoiding the perception of harmful delays for both those receiving care and those administering the healthcare delivery. Efficacious: avoiding waste while providing care that does not vary because of client characteristics (e.g., socioeconomic) or patient threat/attitude (e.g., Chow Chow); ensuring what is needed is recorded in the records, and the client’s response is duly noted in sequence. Client-centered Patient Advocacy: always speak for what the patent needs, and then fall silent and listen to what the client wants. Stressed clients do not want options, they want to know what is needed, now! The traditional good-better-best treatment option logic presented to clients was only economic-based options, not what was best needed for the patient's welfare and quality of life. Stay true to your calling - if you do not speak clearly of what is needed for the pet's quality of life, only the patient will suffer when the client leaves confused. If all veterinary practice owners, as well as facility boards (e.g., multi-practice complexes, multi-doctor hospitals, multi-owner, shareholders, etc.), could use the above Six Targets of Opportunity as an overreaching blueprint for establishing or reviewing their core values, surely clients would experience greater satisfaction and staff could show more pride (i.e., clients perceive staff pride as a quality factor in most healthcare settings). The VCI Signature Series monographs, have a series of planning forms/tools to assist in both core value development and project planning (available at the VIN Bookstore, www.vin.com). Veterinary Consulting International can assist with on-site implementation (expanding the knot-hole); the web site (www.drtomcat.com) shares the various programs and time-based fees. The 21st-century veterinary healthcare delivery should be a staff-maintained and monitored system that provides client-centered, patient advocacy, evidence-based, and system-oriented quality care. All of this can be realized if veterinary healthcare leaders consciously incorporate these aims into the redesign of their Boards and policy/precedent operations. IT IS IN THE PRACTICE CULTURE To facilitate the fundamental changes, the environment in which care is delivered must be considered. Using the aims above as guidelines, the multi-doctor/practice complex administrators should target the following four areas of the facility environment in their Board feedback reporting system: The infrastructure that supports the dissemination and application of new clinical knowledge and technologies. Providing evidence-based care will significantly improve quality . . . to provide such care, the leadership must develop new tools so that referring clinicians can be rapidly made aware of the benefits and adopt the best practices for the patients as standards of care. In a lateral perspective, alternative care techniques are emerging that assist in chronic care . . . local sources need to be identified early. The information technology infrastructure is redesigning healthcare delivery and continuity of care. To reduce errors and improve client confidence, clinical, financial, and administrative transactions must become automated. Most all of the current veterinary software systems are forensically inadequate, but before the end of the decade, most handwritten clinical data could be eliminated by the next generation of software development. Significant progress is being made in Progress Note driven linkages, automated inventory systems, and PDA-type input devices, as well as related tools to ensure protection from forensic liability and multiple entry requirements in the software systems. Payment policies work against practice liquidity. The traditional habit of cash at discharge reduces the perception of affordable pet care. Practices must develop linkages with third-party payment systems (e.g., Pet Insurance, Care Credit, etc.); these systems cannot require discounts or membership fees if practice liquidity is to be maintained. All stakeholders in the veterinary healthcare delivery system must reexamine payment policies to develop methods that provide fair payment for good clinical management of the types of patients being seen. Financial services must be aligned with the implementation of quality care processes of the best practices and achievement of better/faster patient recovery. Preparation of the veterinary healthcare workforce must be a concurrent evolution. Clinical education must be restructured to accommodate the aims of the 21st-century healthcare system, which includes improved client communication skills, team development, outcome measurements, and individual performance accountability. Because systems thinking will be a cornerstone of the transformed veterinary healthcare system, the practice staffs will need client-centered skills to transfer skills and knowledge that are perceived as values deserving of appropriate fee schedules and treatment plans. Management and medicine will become more closely linked, and doctor commitments will drive the elevation of income, thereby reducing the traditional expense percentage management systems. Redesigning veterinary healthcare operations in multi-veterinarian cultures, using these four Board policy and precedent angles, requires a skilled communicator, hopefully with a high EI quotient. This will allow a better chance for creation of a system that uses the best knowledge which is being focused intensely on the best patient care, and that works across the practice's diverse veterinary healthcare providers and delivery settings.
THE EIGHT STEPS TO MULTI-VET PRACTICE SUCCESS 1. Ensure the practice veterinarians sets policy and precedence ONLY between the falls of the gavel; trust in the administrative staff for implementation for outcomes. Hold specific people and groups accountable for improvements in quality or outcomes of care; chart and report on improvements monthly. 2. Devote as much time to reporting quality issues at professional provider meetings as you do to financial issues. Focus on the environment and policies needed for selected outcomes that mean most to the patients, clients, and the community. 3. Base a portion of the top management team’s compensation on achieving quality and outcome objectives, not just on achieving financial goals. 4. Ensure the stakeholders have a basic understanding of Continuous Quality Improvement (CQI) criteria, and ensure each team member has CQI in their own development plan to assist in the community outreach commitment associated with being a practice leader. 5. Ensure the operational budget promotes CQI in the continuing education expectations by providing specific opportunities to increase the quality and scope of veterinary healthcare services being offered. 6. The team members start to play a more active role in researching and securing the needed information to upgrade information systems. 7. The healthcare team works with external groups in the community and nationally to create a more favorable referral system and professional community environment. 8. Ensure the entire team has an operational focus on a clear set of core values (ALWAYS inviolate) and mission focus, so if any team member starts to represent themselves instead of the combined practice entity, there are mechanisms for replacement established and the leadership initiates implementation immediately. Multi-doctor, multi-owner, and/or multi-practice veterinary complex Boards need to center on removing the barriers of “old thinking” and “old paradigms” as they pursue healthcare governance systems that have proven effective. In the text, Building the Successful Veterinary Practice: Programs & Procedures (Volume 2), Blackwell/Wiley & Sons, chapter 1, describes some of the new paradigms for success in the new millennium: It was not cost containment - it was increased productivity! It is not staff recruitment and training - it was staff retention and recognition! It is not “within the job description” - it is exceeding expectations It is TRAIN TO A LEVEL OF BEING TRUSTED, not just good or okay. Don’t respond to the competition - instead meet unmet needs It was never guest relations - it is client-centered service & patient advocacy It can never be “recommendation” - it must be “needs” It is not about assigning blame, it is about giving credit and recognition in a public forum; savvy leaders understand shortfalls are just reflections of their own poor training programs. It should never be gross income - it must be net remaining in the end! It is not "me", it is "we", "us", "our"; always together to common outcome targets and duty zone objectives.
When a management group makes quality healthcare delivery the imperative, and invests in developing the practice/facility culture by collaboration with the professional staff, the entire veterinary complex entity starts to become systems-oriented rather than process-oriented. Practice owners fall short when they are unable to translate modern knowledge into practice, or to apply new technology safely and appropriately concurrent with new third-party payment modalities. The practice leadership must address the policy and precedent of the healthcare complex (not operations), and monitor the fiscal well-being of the veterinary healthcare entity (not Average Client Transaction); they must hire the right people for top administrative jobs to ensure implementation expertise is available on a daily basis (never do it themselves). The appropriately skilled veterinary healthcare administrator, with a clear set of practice-developed core values and mission focus in mind, leads the creation of the operational systems that: eliminate rework, eliminate the risk of error, and eliminate uncertain accountabilities. Concurrently, the administrator must be constantly striving to heighten client satisfaction, increase professional fulfillment, and foster strong/effective veterinarian-nurse partnerships in patient care. If you want a hands-on opportunity to assess your EI, I recommend a watching for courses at your local hospital on "mindfulness". Most mindfulness courses are designed to assist leaders in becoming purposefully aware of his/her thoughts, feelings, and decisions in the present moment, non-judgmentally. It serves as a pre-requisite to developing self-awareness and personal wisdom. Try to stop your immediate responses in a discussion setting by taking a long inhale, and then a slow exhale, before repeating the person's statement/position in common terms. This should derail any hijacking or refocus efforts common in a vet-centered practice setting. | ||||||||||||||||||||||||||||||||||||||||||||||||||||